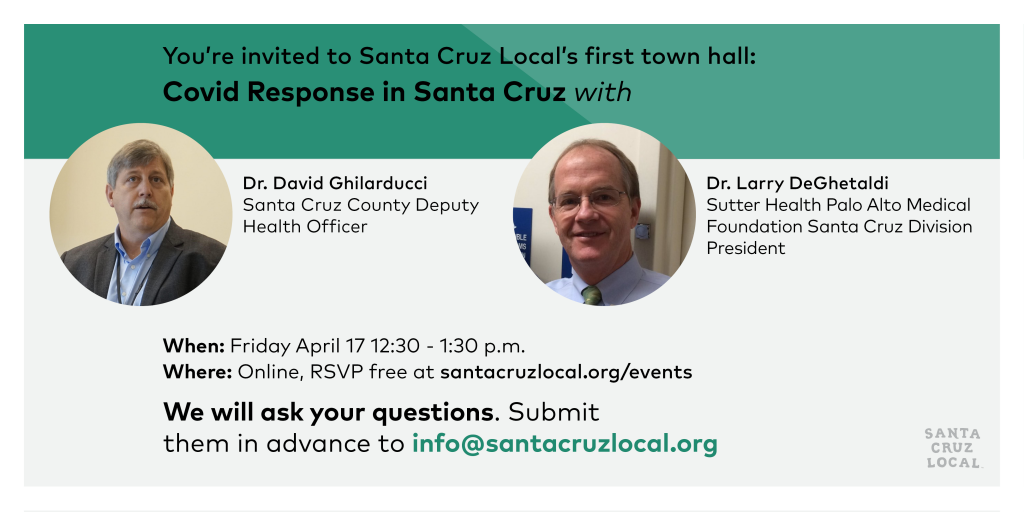
Santa Cruz Local hosted its first of several town hall meetings Friday, April 17 on Zoom. Our guests: Dr. Larry DeGhetaldi, Sutter Health Palo Alto Medical Foundation Santa Cruz division president, and Dr. David Ghilarducci, Santa Cruz County’s deputy health officer.
Some takeaways: Santa Cruz County can maybe expand to 60 intensive care beds, but models predict 100 will be needed at a peak in May or June. The plan is to transport patients to hospitals out of county. Dr. Ghilarducci said the shelter-in-place orders are a blunt but effective tool – and he expects it to last until the county has broad, widespread testing. Meanwhile, the local hospital system has lost most of its revenue since hospitals have cut elective surgeries. Some front-line workers have seen cuts in pay.
Listen to the full town hall video call, where Santa Cruz Local co-hosts Kara Meyberg Guzman and Stephen Baxter ask your contributed questions.
- Attend Santa Cruz Local’s members-only solutions meetup 8 a.m. Tuesday April 21.
TRANSCRIPT
Transcripts are usually only available to members. We offer coronavirus-related transcripts free as a public service.
Can we count on you as a supporter of public service journalism?
KARA MEYBERG GUZMAN: Thank you so much to everyone for coming.
We’re your co-hosts Kara Meyberg Guzman and Stephen Baxter.
We’re lucky to have on our panel today Dr. Larry DeGhetaldi and Dr. David Ghilarducci. We’ll introduce them in a second but first a little primer on how this town hall works.
We will ask your contributed questions. Many of you emailed them ahead of time. If you have questions, you should see a little chat box on the right-hand corner of your screen. You can type them there. Natalya Dreszer, our staffer behind the scenes, will take your questions and feed them to us.
Before we get started, I also wanted to let you know we have a membership drive going on right now.
Santa Cruz Local is a local news podcast, newsletter and website. And we give you the deepest coverage on local government. Right now, we are supported largely by memberships from people like you. Natalya will put the membership link in our chat box so you can click it to learn more. Also, let Natalya know if you’d like to get on our email newsletter it’s free.
Stephen are you there? OK. Well I will go ahead and do the intro. Again, we’re joined by Dr. David Ghilarducci. He is Santa Cruz County’s deputy health officer. He’s part of the leadership team at the county that’s driving the healthcare response to the coronavirus. Fun fact about Dr. Ghilarducci, he was a firefighter and a fire captain in Santa Cruz County for 16 years before medical school.
And our second guest is Dr. Larry DeGhetaldi. He is the Sutter Health Palo Alto Medical Foundation Santa Cruz Division president. Fun fact about Dr. DeGhetaldi, in 1974 he was the captain of UC Santa Cruz’s soccer team. Before a game against UC Davis the team voted to change their name from the Pine Cones to the Banana Slugs. This predated the official mascot of UCSC, the banana slug.
Dr. Ghilarducci and Dr. DeGhetaldi, welcome!
DR. LARRY DEGHETALDI, DR. DAVID GHILARDUCCI: Thank you. It’s good to be here, thanks.
KMG: So, first question, for Dr. Ghilarducci. You said this week that projections show that our county will need 100 ventilators for COVID patients when we hit our peak. We have fewer than 50 ventilators right now. What has your team done this week to try to get to 100?
DR. GHILARDUCCI: Well, thank you for that question. It’s probably the one that keeps me up most at night. We are having continual discussions with our health care leaders about any creative ways that we can expand capacity. The number of ventilators is just one part of the equation though. The other part is having the people to staff those. So, there are opportunities to bring in staff through the California Medical Corps. … especially folks that manage ventilated patients. So, this is going to require quite a bit of a resource. We are also investigating all of our options in terms of moving patients out to where ICU beds may be available elsewhere. So, kind of a multipronged effort that looks at expanding local capacity, bringing in help and maybe moving patients to where there might be more capacity.
KMG: Just to follow up on that for a second though, it seems like the last two weeks we’ve stayed at 50 ICU beds. Do you see that surge, max surge capacity increasing at all? Is there a chance that that number can move upwards?
DR. GHILARDUCCI: You know, I’m not seeing a whole lot of expansion capacity left beyond the 50 that we have. We might be able to add another five or 10 in sort of really extreme circumstances and that may happen. But much greater than 50 is not likely, in my opinion, at this point.
So, we’re going to you know, probably focus more on trying to find other places for these patients to go. Fortunately, we have a pretty robust transportation system with ambulances and a helicopter that’s based here in Santa Cruz County that can help us move these critically ill patients.
KMG: Another follow up for Dr. Ghilarducci. Your team put up this chart at a county supervisors meeting this week and it shows the projections of intensive care unit beds needed in the county. Can you explain this chart to our audience? And how does the county use projections like these to make decisions on shelter in place orders?

DR. GHILARDUCCI: Absolutely. Let me answer the second part first, about decisions on shelter-in-place orders. And I think this is a key concept for your readers, but also for the country as a whole, is that shelter-in-place orders are a direct result of not having testing capacity.
And that is a worldwide issue but also a particular issue here in the United States. Testing capacity is about having the machines that can run the tests, but also having the reagents that the machines requires. It’s about having the swabs that you need in order to obtain the sample and having the PPE for the people that are doing the, the administering the test. SO that they’re protected. And we have shortages in all of those areas.
But testing capacity is building, and we’re looking at some creative ways of expanding capacity. Looking at all of those elements that I mentioned. When we have a better idea of who is infected and who is not – then we can be more selective in terms of how we isolate. But right now, we have a pretty blunt tool which I have to say has been pretty effective, especially in Santa Cruz County. We have one of the slowest rates of growth in our county, largely as a result I think of a responsive population here.
I think the, the early action that our health officer Dr. Gail Newel made, has been tremendous. The Bay Area Health Officers in general, and California in general, have been pretty aggressive about that. Had we waited another week, we might be seeing a far different picture today than we are. So, as far as the graph that you showed, the one that you had up was actually hospitalizations. There’s a different bed that looks at ICU beds. But hospitalizations I actually feel a little bit better. The statewide projections that they have for Santa Cruz County predict possibly up to 300 patients at one time will be hospitalized with COVID. But and our hospital capacity is probably closer to 400. And that is largely the result of Dominican and Watsonville and Sutter doing some creative ways of expanding their inpatient capacity. That’s for hospitalized in general.
But for the ICU, as we said before, there are some functional limitations that will be very difficult to get beyond. So, we’re looking good as far as hospitalizations right now. Obviously, if you look at this graph, you can kind of see a dark blue band, and then a light blue band, and those represent, and not to get too technical, but those represent the kind of odds of where we think it could be. The light blue band represents a, what’s called a 95% confidence interval, which means that there’s a 95% chance that we’ll be somewhere between those light blue bands.
And then the dark blue band is a 50% chance of being within there. So, the projections going forward, at least until the end of May, look like we have capacity, but getting beyond that the numbers get much more uncertain.
STEPHEN BAXTER: I had a question for Dr. DeGhetaldi. If you can hear me. Thank you for coming, first of all. We were sent a document this week that showed Sutter Health workers on the front lines, some of them are no longer receiving hazards and overtime pay, and I was just wondering what Sutter’s doing to fix that. The question came from a listener.
DR. DEGHETALDI: So, all the health systems, most health systems, individual providers, have seen patient volumes drop by, you know, 50 to 80%.
And for our employees, we’ve kept most of our employees on. But as volumes and patient demand for traditional ambulatory services drop – this is not true… this is true for all health systems, typically when a hospital has a low census, we call patients off, they retain benefits.
What we have seen is we’ve asked employees to take some PTO. We have some emergency funding available for full-time staff to cover. But what we’ve largely seen is we’ve asked the entire workforce to decrease some. And so, I don’t really understand the question. We’re trying to preserve access to benefits and keep people working as best as we can. We’ve seen a huge shift from face-to-face patient work to virtual patient work, and that’s occurring all over the country. And I’ve been very impressed by the US healthcare system’s rapid movement supported from payers from the federal government to private insurance companies supporting the movement from traditional face to face care to virtual telephonic video visits.
SB: And a question for Dr. Ghilarducci, we had a question from a Santa Cruz Local member, Jonathan Coleman, he asked what is being done to protect farmworkers. Can the county use its authority to improve health and safety conditions in migrant housing, transportation and work, to and from the fields?
DR. GHILARDUCCI: Excellent question, and thank you for that. There are a number of efforts directed specifically to the ag community. And we know that they are an at-risk community for a number of reasons, access to primary health care being one of them. Living in closer kind of settings. The kind of transitory nature for some of these folks. I’ve also heard a report last night that there’s a bit of an outbreak going on in Tijuana. And my colleagues in San Diego and Imperial counties are seeing some evidence of that. And Mexico in general. I think there’s’ a real struggle going on down there.
So as far as outreach, we are working with Salud Para la Gente with their efforts to reach these groups. We have multilingual, bilingual education going out. We’re having discussions now about building testing capacity for that group, to specifically focus, and you know, right now the testing that we do have in the county, which is limited, as I’ve said before, is kind of passive. That is, we’re waiting for the patients to come to us and then they get tested. And I think that we’re going to have to shift to more community surveillance, that includes going out to people and testing them where they are providing broader resources that don’t require them to go to the doctor or the hospital to get tested.
So multiple areas, it’s an area that we recognize as being a potential hotspot. And you know, there’s a lot of work been has been done in that area.
SB: Can, can I ask, Kara, just real quick, a follow up for Dr. DeGhetaldi? Since we’ve haven’t heard as much from the Sutter end of things as we have from the county. Can you just give us a little overview of where Sutter is at in terms of the COVID response? I mean, as one of the basically three major hospitals in the county. What are some of the big challenges there that you’re facing right now?
DR. DEGHETALDI: So, you know, and I can speak. There are three large healthcare systems in Northern California, and they’re all in Santa Cruz: Kaiser, Dignity and Sutter Health. And they’ve all responded, I think in similar ways. They early, the system set up incident commands to address the emerging pandemic. And we’re really, as David showed on the graph, we’re really focusing not so much on how many patients are positive COVID in a community, but what’s the experience in the ICU and what’s the experience on the inpatient side?
Because that’s really the best measure when we don’t have adequate testing. The best measure of how significant the impact on any given community is, is going to be how many patients in the ICU? How long are they in the ICU? What are their outcomes and what are we doing for those patients?
So in for us in Santa Cruz, we like other healthcare systems rapidly pivoted. First of all, we stopped doing elective procedures. We stopped doing elective standard ambulatory visits, you know, health maintenance, preventive visits, to protect patients from to allow patients to stay at home.
And then we, as I said, we moved as quickly as we could from the traditional physician office visit to virtual visits. And that and I’ve been really surprised how quickly we’re able to do that. We set up respiratory clinics very early. And in fact, the first Santa Cruz County patient diagnosed with COVID was in one of our respiratory clinic visits.
And, you know, the community’s come out and folks are bringing food to our respiratory clinics to, to help our workers. They’re working out in hail, and then rain and, you know, testing patients in their cars. It’s, it’s been, it’s been amazing to see. And it’s been amazing to see signs in the community, thanking our heroes, you know, for the healthcare workers. And so. It’s been a – we’ve seen a generation of healthcare change in six weeks.
KMG: Dr. DeGhetaldi, can you talk a little bit about the economic situation in our hospital system right now?
DR. DEGHETALDI: Yeah. So, the, the American healthcare system, you know, we there’s many different payers, from MediCal to Medicare to third-party payers. The most, the health of the US healthcare system relies on elective procedures, really to, in a way subsidize other kinds of services and health plans. Those have all stopped – the stuff, the bread and butter stuff of the US healthcare system.
And so what we have seen all across the country, and it’s particularly hard on, you know, single hospitals in rural areas or solo physicians anywhere, the lack of inflow of, you know, the funds that that sort of subsidize, all the good works that they do, have stopped.
The federal government, part of the CARES Act released $100 billion and $30 billion has been distributed to US healthcare providers. It’s more than a drop in the bucket, but it’s not enough to keep the systems whole.
We’re fortunate to have well-run federally-qualified health centers If that have the funds to, you know, to stay open over the next few months. And the three healthcare systems are, you know, continuing to support the care to our community. So, we’re OK for the time being, but this can’t go on forever.
KMG: You talk about the local situation. I mean, are what’s happening in Santa Cruz County? Have you heard about furloughs of health care workers? You know, we’ve heard about what’s happening from Sutter and, you know, frustration about that.
DR. DEGHETALDI: Well, there will be some slowing down of, you know – we’re not calling folks in as if we were. Look, we’re, many of the systems are down as I said, you know, 60 to 75%. So, each system and individual provider office and community clinic is they’re trying to find the best way to protect their, their patients and do the right thing by their staff. So, it’s varied. But not everybody is working full time.
SB: I can ask this next question, Kara, from a listener.
Maybe this is for Dr. Ghilarducci. And how many Santa Cruz County deaths does the model predict by May 1? There have been two deaths so far. And I’m curious if either of you are surprised by that figure.
DR. GHILARDUCCI: I can say that. We don’t have. Our epidemiologists right now we’re working on those projections. I’ve asked for those yesterday to get a better sense. Their, their early projections were, were pretty high. I can’t give you a number off the top of my head but I don’t have much confidence in those very early projections. I think the newer ones will give us more data.
Am I surprised by the two [deaths]? I think the – at this point we had expected actually more.
These people when they, when they’re sick like this are in really dire straits. And this particular virus is really kind of, you know, we’re all scratching our heads about this one. People can sometimes have very mild illness. Sometimes they’re not even aware that they have the illness.
And then sometimes they can feel a little bit ill and then they rapidly decline. And there’s this kind of odd trajectory for some people that we’re still trying to understand more about.
So, to answer your question, I, I’m not surprised by the two that we’ve had. There may actually be others that we don’t know about. And I think the other concern that I have is that we’re seeing an overall decrease in the number of heart attacks and strokes that we would normally see this time, you know, over a course of time. And I suspect that those things are still happening, but people are not seeking care.
And there is capacity in our hospitals. We have, you know, cardiologists that are standing idle. We have neurologists that are ready to take care of people. And if you have a medical emergency – I know people are worried about going to the hospital and they’re in there thinking they’re going to get infected there. But if you have a medical emergency, like a heart attack or stroke, the time is of the essence that you get treated. And the best thing to do is to come in. So, so yeah, two deaths. Tragic. And, you know, very sad. I do expect more. I think we’re doing better than I had thought. But I think that there’s some undercounted collateral damage that’s happening too.
DR. DEGHETALDI: Could I comment, because you’re being a little humble, David. Um, the two deaths are terrible. But we’re sitting right next to Santa Clara County, which has a lot of cases.
We really expected a lot worse and your boss’s early sheltering order – and we’re a little bit protected and isolated geographically plus the patients that we have in our community don’t suffer from a lot of the comorbidities that that many communities suffer from.
It’s not luck. But you’re doing – public health deserves a lot of credit. And so just take it, take it. You know. So, it’s – two deaths are terrible, but we thought, a month, three weeks ago, with your graph, we were looking at that and not sleeping.
DR. GHILARDUCCI: Thank you.
KMG: I have a question from Santa Cruz Local member Ron Goodman. Santa Cruz County has reported about three to five new COVID cases a day. Does that show the limits of testing? Or are there actually three to five new cases a day? And also, can you explain – he’s asking for some explanation of – why is the peak – explanation of why the peak is pushed back till June?
DR. GHILARDUCCI: OK. I’d be happy to take that one. So yeah, about three or so a day is about right. And again, this is just the people that have been tested and tested positive. We do have probably a one to 10 ratio of tests to positive. So about 90% of the time when somebody is tested, because they have symptoms. Sometimes they’re tests when they don’t have symptoms, but 90% of the time it comes back negative.
With regard to that, that, I want to say that the test is not very accurate when you don’t have symptoms, there may not be enough virus available on the swab to actually detect. So, we don’t recommend that asymptomatic people – people that have no symptoms – get tested because the test. It’s not just a matter of wasting a test, but it’s about providing information that might be falsely reassuring. Because you, you may actually have a virus and it wouldn’t be picked up by the test. So, the test is not useful unless you have symptoms.
So that said, we’re probably obviously we’re not counting the entire population. And there’s more virus out there than we’re counting. So. So we operate on the assumption that if you do have an illness that it’s presumed to be due to COVID. And all of the self-isolation, the quarantine measures that we put in place are super important.
And so, we’re asking people, not to come to work, We’re – we have sick leave policies that we’ve implemented for public safety folks, and for our health care providers that I think have been effective.
We’ve seen some infections in our healthcare community, roughly. I think about 17% have been in health care providers. But when we really dig down to it in our public health nurses do contact tracing and they realize that only one or two of those were related to their occupation, that the exposure came from the community as a whole and not from, from the hospital or from the healthcare setting.
And I apologize there was a second part to your question regarding the rate of rise?
KMG: Um, yeah, I’ve – we’ve heard this from actually a few questioners wanting to understand why the peak may be in June. Like why do the models still show, you know, this big rise in June given all the success we’ve had and flattening the curve?
DR. GHILARDUCCI: Yeah, great question. So yeah, I would caution people, you’ll hear the president, you’ll hear New York, you’ll hear the LA Times report, that they appear to be at the peak. And the thing is with, with those reports that you hear those numbers, like sort of nationwide, or even statewide numbers are driven by large population centers, which we’re not. So that’s not necessarily representative of Santa Cruz.
Also, our, our rate of rise has been much lower than, than the rest of the country and the rest of California. So, there’s something special about Santa Cruz that has helped us flatten the curve.
But flattening the curve is a good news, kind of bad news thing. One is, flattening the curve reduces the height of the peak, meaning that we’re more likely to be able to have capacity for when that peak kits, but it also pushes that peak farther out and down.
So, so it’s sort of imagining a marshmallow that you’re squashing down on and it kind of spreads out. That’s the idea of flattening the curve.
SB: Just to follow on that it’s for the lay person, it seems like that peak goes out further than the shelter order goes out further. At what point do we find these models are not as good as we thought? And it seems like those two things follow each other. Can you talk about when that stops?
DR. GHILARDUCCI: Yeah, right. Well, I’ll tell you what- It stops when we have testing. And the shelter in place is, as I said earlier, is a blunt tool for the – that’s a complete reflection of the lack of testing and testing, testing capability.
So, you’ve seen other countries like South Korea have been able to relax their shelter-in-place and isolation restrictions because they have a good sense of what’s happening. So, we’re in the phase right now where the only tool we have is to do what we’re doing. A
And fortunately, it’s working but it does have side effects, economic side effects and social side effects that that we’re completely aware of and are trying to balance that. But once we have a better idea of testing- when we don’t have to wait a week for a test result to come back, then we can jump on the little outbreaks.
We’re going to see, you know, right now we’re sort of seeing the big wave, then what we’re going to eventually get to is this sort of period of little ripples, or little clusters that happen and then we can react to those clusters. We can do more targeted isolation or sheltering. We can do some, maybe some half measures to, to tamp down those little ripples that come. But we can’t detect the ripples without testing.
SB: I’m just one quick follow. When do you foresee, Dr. Ghilarducci, elective surgeries? I mean, and I wonder if that’s been a big conversation with people like Dr. DeGhetaldi and other medical leaders.
DR. GHILARDUCCI: Yeah, I’d like to hear from Dr. DeGhetaldi on this as well but you know, people have, you know, medical needs that go beyond COVID, of course. And, you know, we’re, we’re – our healthcare providers are worried about people with – that need cancer surgery. We’re worried about maybe making sure that mammograms are happening. That we’re not, you know, we don’t – we’re not blinded to all the other medical issues that people have and some things. There is a cost to putting those off. And so, we’ve actually had conversations and again, I’ll let Larry chime in. But we’ve had conversations about maybe allowing some more kind of elective cases to go through.
DR. DEGHETALDI: Placer County opened or made a recommendation, I think today or yesterday, that elective surgeries could go forward. We’re being really cautious with that. And, and so, no, we’re not doing elective procedures now, but we’re certainly planning for when we start to do it, to do it as safely as we can for patients and staff that work in positions.
But David’s point about mammography. We identify breast cancers, not daily, but all the time through screening mammography. That’s not happening. And colorectal screening, colonoscopies, they’re not happening.
So, there are, there is a cost for not doing the basic preventative work that we are, that we excel at in this county. So, we’re looking at not just, you know, your elective hernia operation, but when do we start immunizing children and doing pap smears.
So that’s what, we’re talking about all of these things.
KMG: Dr. Ghilarducci, you said that testing is the limiting factor to when we can see a significant easing to our shelter-in-place rules. I guess, what hope do you have with the three new testing centers that opened locally this week? What kind of solution is that and what more is needed?
DR. GHILARDUCCI: Yes, thank you. Those are all a step in the right direction. Those are intended for the patients that are, that seek care at those facilities. It’s not the kind of, sort of outreach kind of testing that I described earlier. But they are a step in the right direction. You know, before, before we had local testing capability, we were relying on the Santa Clara Public Health lab. All of these had to be shipped over. They were very gracious to accept our specimens and to do our tests. But they obviously are running into capacity issues too in Santa Clara County.
We also had commercial labs that have come on board in the past few weeks, but they have really struggled with the, with the loads. And we’ve heard reports of one-week turnaround times, which almost becomes useless. You know, a week is like a year in a pandemic because of how spread can happen while you’re waiting.
So, so we have a lot more to do. We’ve had some interesting offers from researchers at UCSC who do genomic testing, and they can do, they can build a PCR test. And so, we’re investigating that.
We’re looking at some foundational, some large donations to help us build capacity. So, you’ll be hearing more from us as this goes.
SB: Just to follow up on the testing. I mean, in Santa Clara County, I know there’s a lot of comparisons but they’ve had roughly 15,000 tests. Our county I believe around 2,500 tests from the beginning. Is Santa Cruz County getting short shrift with tests? Because it sounds like they get sometimes short shrift with PBE and – sorry, protective personal protective equipment – and other requests because our county is not as populous as others. Is that part of what’s going on? And does that ever change?
DR. GHILARDUCCI: I think it is part of what’s going on. You know, I think we’re in a situation right now where, where we don’t have a leadership role at the federal level. And so, the states are competing with each other for resources. And just anecdotally, I can tell you that we had a modest order for testing materials that the vendor said they were going to send to us. And then they told us, uh, we have another priority. You guys are lower on the list. And so that is part of it is we’re not you know, we’re not LA County. We’re not New York City. And so, we are a lower priority.
DR. DEGHETALDI: Let me just – it was very, very difficult for our frontline physicians in the first few weeks of this this crisis to not have testing or to have very, very limited testing and to follow the CDC, very strict guideline.
Testing criteria have opened widely. We are getting results back within 24 hours, and in some cases, 12 hours. Some of our organizations have point-of-care testing, although the reagents are limited there. That’s the Abbott test I think somebody’s asked about. And don’t confuse this with serological testing, which is still more theoretical. It is available, but we really don’t know how to interpret a positive serological test – whether it confers immunity, or how certain it is that you did have COVID.
So that’s another part of the technology that we really need to really develop and spread.
KMG: Dr. DeGhetaldi, it might be interesting for listeners to hear a little bit about the conversation we were having offline ahead of this meeting. We were talking about the Stanford study that came out today about antibody prevalence in Santa Clara County. And just curious if you could share your big takeaways from that study.
DR. DEGHETALDI: Yeah. Well, I haven’t seen a published report. So, it’s a little bit preliminary. But our infectious disease. One of our ID docs says Stanford has, Stanford has the capacity to do the serological testing looking for antibodies in the patient’s blood to COVID-19.
And in many parts of the country, we’re trying to understand how widespread is this infection which can be asymptomatic in so many cases, right?
So, in Santa Clara County, Stanford ran a little over 3,000 random tests. And they’re seeing a likely prevalence in the virus, in the less than 4%. Maybe as low as 2%.
So, what the, our first reaction to that is? Not much, not much herd immunity there. Right?
So, what does that mean, as we go forward? More and more testing is needed. We need to understand this thing that we’re fighting.
SB: Yeah. Let me just ask a follow up, again, kind of from the layperson’s perspective, does that mean that there’s some type of strain that’s different on the West Coast that that was different from the East Coast or no? Because I think it was talked about, Dr. Ghilarducci, earlier, that things are happening differently in New York than they are here. So, does this study seem to suggest that people possibly could have been infected with a different strain and/or is that less severe than what’s happening on the East Coast? Or does it even speak to those things?
DR. GHILARDUCCI: Yeah, thank you for that question. Um, yeah. This came up the other day. So, this, the coronavirus is an RNA virus. It’s a type of genetic material that can actually mutate pretty quickly. So, we know that there are different varieties of the coronavirus circulating around. And they can actually be traced from where they came from.
And what we saw, the studies have shown in New York, that mostly it’s of European origin in New York City. So, the virus was circulating in New York and was brought in from that direction.
In the Bay Area we’ve seen actually a mix. There was one genetic code that looked like it came from a meeting in New York. So, we actually got some virus from New York that came here.
Others probably came from Asia and other places like that. So, we think there were probably multiple sources of virus that were brought in from multiple different places into California.
We think this was probably happening throughout January. And, you know, we obviously travel we was restricted in in mid- to late- January, probably, you know, the horse had already left the barn at that point.
KMG: Here’s a question from Davenport resident Noel Bach. She wants to know with the beach, with the beaches now open, would it be helpful for Santa Cruz County leaders to consider following San Mateo County’s lead where they only have beaches open to locals?
DR. GHILARDUCCI: Yeah, there’s I’ve been hearing a lot of concern from people about Santa Cruz becoming a magnet for everybody else who doesn’t have beaches to go to. And obviously, we’re, we’re, we’re a tourist destination for most of California.
And I can tell you that it’s a tradeoff that the health officers had to make in terms of reopening the beaches. She recognizes the value of open spaces. She’s, you know, considered the kind of risk scenario of being out in an open area with maintaining social distancing and all the things that we’ve done before that. And, and then we also have mechanisms in place to have to, you know, shut them back down if we see an issue.
So, all of the things that we, that have shown success prior to the closure last week, the, the flattening of the curve, the increased doubling time for the cases, etc., will continue to be in effect.
And so, we have some confidence that we’re managing that tradeoff OK, but there’s going to be a close monitoring of that.
SB: Another question from a listener, which we just got, I think, which is pretty cool. One of them says, if the tests aren’t reliable for people without symptoms, how will we ever get to sufficient widespread testing? And I think you talked about this a little bit, but could you elaborate, either of you?
DR. DEGHETALDI: Well, the public health officer should go first, I think on this, I didn’t comment on serological testing, which would demonstrate prior or even distant infection, so that that’s an important tool. But, David.
DR. GHILARDUCCI: Well, no, Larry, you’re, you’re an expert in this as well. I think the serological testing has some promise. We don’t know enough about it yet.
So yeah, the I think if we were able to focus the testing, broad widescale testing on people that are symptomatic, then we’ll get a much better sense of what’s, what’s going on.
If, the test is not very good on people that are asymptomatic, and so, you know, it’s going to, it’s going to require people to be aware of their symptoms to, to respond to that to act responsibly if they do have symptoms.
You know, cloth facial coverings have been an important aspect of this. These are, you know, a cloth mask, I don’t want to use the mask the word mask because that’s really a medical grade term and that’s intended for healthcare providers.
But the cloth facial covering is an excellent way to reduce the risk of you infecting somebody else. It does not provide a whole lot of protection for the mask wearer from other people.
And probably the most common way that the virus will be passed is from your hands to your face. And so, handwashing is, it sounds so pedestrian, and so low-tech but it actually is one of the most important things.
DR. DEGHETALDI: The dilemma here is the swab tests for the presence of the virus. So, you have to have sufficient virus present. You can’t culture viruses like you can strep, a bacteria.
And the serological test is a blood test not looking for the virus in the body, but the, our own antibodies to the virus and we can usually tell whether it’s a recent or, or a more distant infection. So, viruses are harder to track in the in the community.
KMG: I just wanted to remind our listeners that you can submit your questions in the chat box at the bottom of your screen, on the on the black bar, you’ll see chat and then you can type in your questions there and we’ll read them. This question is from Santa Cruz Local listener Dana Bagshaw. She does not have a car but she feels that she needs to get tested. What does she do?
DR. DEGHETALDI: Well, I can answer for the two respiratory clinics and PAMF. They look like drive thru but we are testing folks, I don’t know if we’ve tested somebody coming through on a bicycle but we are testing folks that walk in. And many think of Manhattan, they’ve had to solve that, where so many people don’t have cars.
KMG: Dr. DeGhetaldi, can you speak about the situation at Sutter Maternity and Surgery Center? I know you’re no longer doing elective surgeries, but also our hospitalization COVID caseload is you know about less than a dozen right now county wide. What’s going on at the surgery center and are you taking COVID inpatients there?
DR. DEGHETALDI: No. The answer is no. But we have, working with Dr. Newel and Ghilarducci, we have worked with the other two hospitals for what we call surge planning. And so, we’re trying to anticipate at any point in his graph or curve, what role each hospital and future alternative care site would play.
One of the messages though that we are all three hospitals are trying are really trying to share with the community is that we are being very careful for non-COVID patients that the hospitals are safe for deliveries.
And that’s an important message that all of us are trying to share. We’re being very, very careful for routine, for standard obstetric services. Very important.
SB: Looking for more questions people. Kara, do you have one lined up?
KMG: Sure. Um, well, I guess this could be a question for Dr. Ghilarducci. This is a question from Santa Cruz Local member Craig Chatterton. Have you heard of any? So, it seems like you know, with such little happening right now, you know, our streets relatively open. Yeah, I guess is, is there more that could be done to – I guess take advantage, actually sorry. Never mind, that might not be a question for you. This question is from Ron Goodman. Some community groups are suggesting that while there’s so little car traffic, and so much pedestrian and bike traffic, that it would make sense to limit cars on some roads. Oakland’s doing something like this. Could Santa Cruz also consider similar restrictions?
DR. GHILARDUCCI: Yeah, thank you. I, I don’t know if that is a kind of a health officer jurisdiction. But I’m all in favor of fewer cars on the road and more walking and more bike riding. And, you know, it’s kind of maybe more of an urban planning kind of question, but, but it’s been if there was any positive to all of this, it’s been that the traffic in the county has been a lot better than it normally is. And I see a lot of roadwork going on right now. They’re working on traffic signals and so forth. So, they it’s a good opportunity to get some of that done.
SB: One question for Dr. Ghilarducci, can you talk about how the county ways public health concern with the economic engine of the county because obviously there’s a lot of people out of work and a lot of business. People who are fretting right now, can you talk about how you weigh in those things?
DR. GHILARDUCCI: Yeah, that’s, that’s a great question. And there isn’t. I mean, it’s, it’s a matter of concern. Our focus is on, on health. And so, we, you know, certainly prioritize making sure that we control the spread of this virus to the extent that we can.
But we recognize that there are tradeoffs. And, you know, some of the tradeoffs I think, Dr. Newel, you know, acknowledged by relaxing the beach restriction orders, recognizing that we still need to go outside, we still need to do healthy activities and so forth.
From an economic perspective, we are looking for any way that we can to, to, to, you know, get back to normal. And so, you know, if we, if we again, have good testing, I think that we can start looking at having people eating in restaurants, again with some appropriate spacing, engineering controls that can happen as far as reducing risks, and maybe get some of these, you know, important kind of activities back going.
But right now, I think the cost of doing those things without the ability to surveil the evidence of the prevalence of disease will outweigh any short-term economic benefit at this point. So, it’s trying to try to make that tradeoff. So, it, do we have a formula or some kind of algorithm that we use? I think, I can’t, I can’t say that. It’s more of a subjective assessment, but we’re certainly have that balance in our minds.
SB: And just real quick, I know the counties working with other counties in the Bay Area to have a unified new, perhaps looser shelter order in May. Would that, could that include restaurants, is that a goal? Or could you describe what we might see in May?
DR. GHILARDUCCI: Yeah, you know, unfortunately, I haven’t had a chance to read some of those proposals yet, so I don’t want to speak out of turn. But, but it would include a kind of gradual and careful relaxation of activities. You’ll probably see a kind of piecemeal relaxation that happens over time.
I would imagine restaurants will be part of that. Are we going to see the boardwalk open anytime soon? Or, you know, are we going to see large weddings and funerals anytime soon? I think that’s going to be much farther out. In fact, that may even have to wait for vaccine, if we have one.
But are there ways to, to kind of go back to normal that can manage the risk? I think that there’s some opportunity there. We’re already seeing, you know, some relaxation, on landscaping, on construction, on outdoor activities. And so that is what we’re going to try to do, going forward.
KMG: This is a question for both of you from Chris Neklason. What is the latest that we know about death rates caused by coronavirus here locally, I guess in this region, including Santa Clara County?
DR. GHILARDUCCI: Larry, I’ve been talking a lot.
DR. DEGHETALDI: Yeah. Um, so let me let me go back a little bit before that. The question, um. It’s incredibly important to recognize that certain individuals are at much higher risk of dying from COVID. And, and I think the more the public understands that, the better.
And I may not rank this in the absolute order. But we know that age is probably the greatest predictor of mortality from COVID. We know that diabetes, obesity, cardiovascular disease, including just regular old high blood pressure, under anything that is immunosuppressing for the patient, patients who are in dialysis or patients with chronic kidney disease, and male gender. Those are all risk factors for dying from COVID. And so, as you think about your individual safety or loved ones, measure that put those on, on the mix.
And we are most definitely seeing those risk factors play out. As David said, we’ve only had two deaths in the county and both patients were older with chronic disease. But those patterns are playing out all over the country, and in Santa Clara County as well.
KMG: Dr. DeGhetaldi, can you sort of speak about that through the lens of the Stanford study and the Dartmouth Atlas study? Like what do we know about we what can you sort of say about that, lethality rates in Santa Cruz County?
DR. DEGHETALDI: Well, I don’t think we can learn anything from the perspective of risk of mortality from the Stanford study.
What the Dartmouth Atlas study that you’re referencing, they have looked around the country at individual communities at measuring how many patients are older, with chronic disease, multiple chronic diseases, and those communities where – and they tend to be underserved and lower income communities in the country – that have lots of folks over the age of 65, with lots of diabetes and high blood pressure, those communities are at much greater risk.
Santa Cruz is a way on the other side of the equation where we, we tend to have even though we have older, a lot of older patients, there’s not much chronic disease in Santa Cruz compared to other parts of the state and the US. So, from that perspective, there’s a little bit of protection for us.
DR. GHILARDUCCI: And I could say that the case fatality rate or the expected mortality of COVID infections is around 2% internationally. And we have about 100 cases with two deaths. So, we’re kind of tracking along that line.
DR. DEGHETALDI: You know, I omitted a big one chronic lung disease. And I’m probably smoking as well, and moderate, moderate or worse asthma.
SB: That was actually one of the questions somebody just asked if there’s a difference between smoker or nonsmoker. So, he’s clairvoyant.
DR. DEGHETALDI: Smart, smart person.
DR. GHILARDUCCI: And there’s, there is a connection between kind of a background pollution exposure to so if you live in a heavily industrialized area that doesn’t have clean air that could probably put you at higher risk.
SB: Yeah, I think we have to do, I want to do I think, one more question. Before we do, I think the last question Kara.
One person asked, Pat Clark, and I’ll sort of adapt his question. We’ve seen, I believe fewer counting fewer COVID cases in South County versus North County. And I just, I wonder if that’s an effect of access to health care or other factors. Can you talk about that?
DR. GHILARDUCCI: Yeah, I wondered the same thing, that slightly fewer proportion. You know, we divided the county into sort of three blocks: north, mid and south. And the fewest number of cases are from the south. I think that there’s a couple of reasons.
One is it’s somewhat proportional to population. Secondly, is we share a border in the South County with Monterey County, and they’ve had some cases from North Monterey County that have cropped up in their numbers and our numbers don’t reflect that.
In fact, we did have a third death in the county that was actually a Monterey County resident.
So, so, but I think access to healthcare is another issue. And there I think is, in particular with some communities, a reluctance to seek health care, because of perhaps immigration status and other issues like that. So, we may be seeing a number of reasons why the numbers are lower and in what in the South County.
KMG: Last question for both of you. We wanted to know if there’s, what you would want people to know, any last parting thoughts.
DR. GHILARDUCCI: Larry, would you?
DR. DEGHETALDI: Well, I think just keep in mind of your own risk factors and the people that you care about. And we’re in – this is not going to go away by May 1. And not by June 1. We’re not going to have a vaccine or an, an effective medication. And that the old-fashioned public health tools are the most important tools we have.
And I hate to say it, but our public health officers are more important than our neurosurgeons and our cardiac surgeons. Suddenly, they’re the captains of the ship.
DR. GHILARDUCCI: I know a lot of neurosurgeons who would not agree with that. But yeah.
I totally echo what there has to say. I, you know, I want to say I’m proud to live here. And I’m proud of my neighbors and everybody who’s responded to this. I think it’s a testament to who we are as a community. Let’s stick together. Think about each other. Some of the acts of kindness that I’ve seen and people have reached out to help others is just tremendous. We’re probably mile three of a marathon at this point. So, I just encourage everybody to keep it up and take care of yourselves.
KMG: Thank you everyone for coming. Thank you so much, Dr. Ghilarducci and Dr. DeGhetaldi. We really appreciate your time.
One quick announcement we have a members-only video chat with Santa Cruz Local over Zoom this Tuesday, we’ll brainstorm ways about how our community can help Santa Cruz County get through this time. Members, you’ll have an invite in your email in the next few days. Bring your own coffee. Hope to see you there.
If you’re not a member, I hope you consider joining. Natalya will put the link in our chat box to learn more about membership.
And for those of you who aren’t on our newsletter, please consider joining. It’s a good way to get, an easy way to get news in your inbox. The link is in your chat box.
Thank you so much for tuning in to Santa Cruz Local and we’ll see you all next time.
Kara Meyberg Guzman is the CEO and co-founder of Santa Cruz Local. Prior to Santa Cruz Local, she served as the Santa Cruz Sentinel’s managing editor. She has a biology degree from Stanford University and lives in Santa Cruz.
Stephen Baxter is a co-founder and editor of Santa Cruz Local. He covers Santa Cruz County government.






