At a news conference Thursday, Santa Cruz County health officials said they were encouraged by the relatively low numbers of COVID hospitalizations in our county. However, the county still only has a maximum intensive care unit capacity of 50 beds. Dr. Gail Newel said she plans to extend her shelter-in-place order past May 3. Santa Cruz Local co-hosts Kara Meyberg Guzman and Stephen Baxter explain their key takeaways from the conference. And they ask the health officials your questions.

TRANSCRIPT
Transcripts are usually only available to members. We offer our coronavirus-related transcripts free as a public service. If you find our work valuable, please consider supporting Santa Cruz Local with a membership.
KARA MEYBERG GUZMAN: Hi! It’s Kara Meyberg Guzman. Did you know that only one person works full time on Santa Cruz Local? That’s me.
We can do so much with our small staff. If you’ve been following our work, I bet you agree. We produce the deepest stories on local government — and recently, the local response to the coronavirus. We want to grow our staff, but we need your help. That’s why I’m inviting you to become a supporting member. About 80 percent of our revenue comes from memberships from people like you.
Our 320 members are the reason we’re able to keep showing up in your inbox and your podcast feed. If you find our local journalism valuable, I invite you to join us. Memberships start at $9 a month or $99 a year. Sign up is at santacruzlocal.org/membership.
[THEME MUSIC]
KARA MEYBERG GUZMAN: I’m Kara Meyberg Guzman
STEPHEN BAXTER: And I’m Stephen Baxter.
KMG: This is Santa Cruz Local.
On Thursday, we attended a news conference with Santa Cruz County health officials. It was at the county’s Emeline clinic. It was the second conference in a weekly series. This week, all the reporters in the room wore masks.
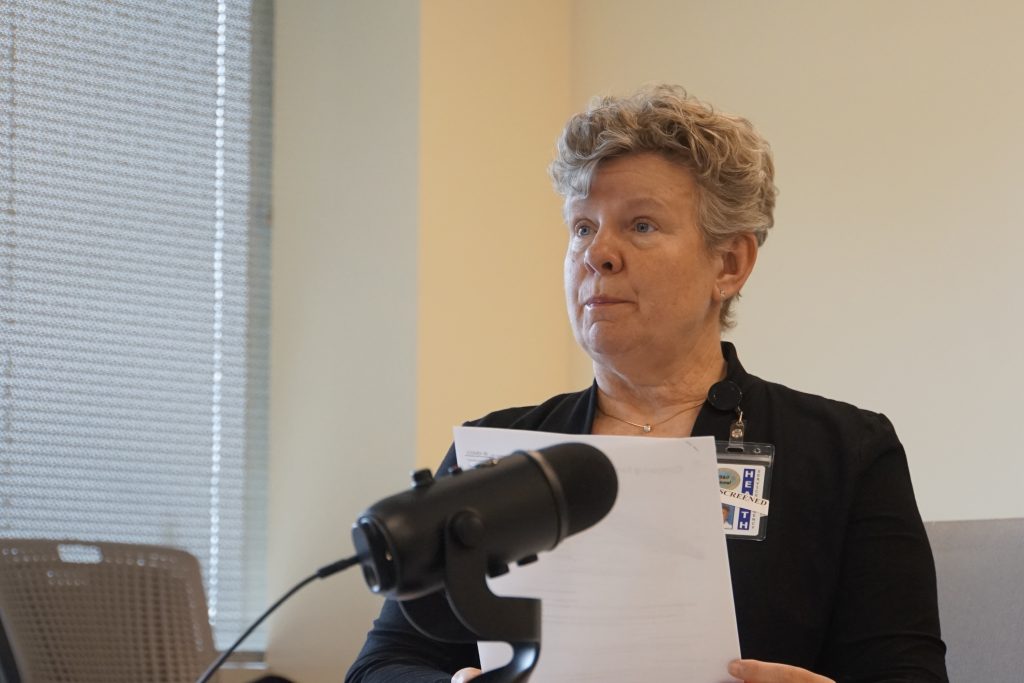
SB: At the conference, we heard from Santa Cruz County Health Officer Dr. Gail Newel, Deputy County Health Officer Dr. David Ghilarducci, and County Health Services Agency Director Mimi Hall.
We’ll give you the top takeaways followed by what we thought were the most useful questions and answers from the conference.
KMG: Also, last week we asked you to send us your questions for the county health officials. We pressed the officials with your questions and we’ll share their answers here.
SB: We had three takeaways. The first, health officials were encouraged by the relatively low number of COVID hospitalizations in our county. As of Thursday, there were 14 people hospitalized with the coronavirus in Santa Cruz County. That’s up from nine hospitalized on April
1.
To give you some perspective, Santa Clara County on Thursday had 278 COVID hospitalizations. Monterey County 16 hospitalizations.
And of course, the number of hospitalizations is relative to the population of those counties. Santa Clara county has nearly 2 million people. Santa Cruz County has about a quarter million people.
A key stat that county officials pointed out was the number of days it takes to double our COVID cases. Thursday, Santa Cruz County had 80 confirmed cases.
County officials look at that number, ICU admissions and other data to form predictions. Right now we have a doubling rate of eight days, according to County Health Officer Gail Newel.
Newel had expected a six-day doubling in our county. So that shows a significant improvement. She attributed that to residents following the shelter in place order
She said it’s encouraging, but she basically, said don’t get complacent.
KMG: Our second takeaway: Our county’s intensive care unit capacity has not changed since last week. We still can only handle a maximum of 50 patients in intensive care. The limiting factors are staff and ventilators.
If we need more, other hospitals, like Seton Medical Center in Daly City, could take our patients Mimi Hall said.
Our county has increased the number of hospital beds for lower-level care. On Monday, county leaders said 1440 Multiversity in Scotts Valley can open as an alternate care site. The Simpkins Family Swim Center in Live Oak also will be a care site. A hundred beds altogether are planned for the two sites.
The county actually delayed the opening of those two sites because we haven’t yet seen a surge of patients yet.
SB: Takeaway No. 3: Dr. Newel said, expect to be sheltered in place past May 3 That’s when the shelter order ends. But that’s also when our county is projected to see a surge in hospitalizations. That’s why she plans to extend it.
KMG: And here are your questions that you sent us. One Santa Cruz Local member asked, if our county had low rates of spread, would our leaders consider installing checkpoints at our county borders to keep visitors out?
Dr. Newel said that’s possible. She said that other counties with limited hospital capacity and a large number of vacation homes have already set up checkpoints. For example in Mono County, near Yosemite, authorities set up highway checkpoints to make sure only locals and those with essential business are let in.
SB: Another listener question: Are we testing everyone in hospitals?
The answer, no. People with symptoms are prioritized for tests, Deputy County health officer David Ghilarducci said. Part of the reason for that, he said, is that if you test someone without symptoms, you’re more likely to get a false negative.
KMG: And a third question from you, our listeners: Does everyone in the hospital receive protective gear?
Not really. The medical-grade protective equipment is prioritized for workers who have direct contact with COVID patients. Each clinic has its own protocols. But generally, workers who are not in contact with COVID patients might use simple face coverings, not medical grade.
Speaking of which, the county only has a small emergency reserve of medical-grade protective gear. The county has distributed nearly all the gear it’s received. That’s 93,000 kits, said Health Services Agency Director Mimi Hall.
SB: OK, that’s our wrap up. The conference started with county health officer Dr. Gail Newel.
DR. GAIL NEWEL: Morning. Thank you for those who are here in person and maintaining your physical distancing, almost. [LAUGHS] I’m going to wait for you to move 6 feet apart.
And for those of you who are calling in remotely or connecting remotely, a special appreciation for you and your efforts for your ability to maintain your physical distancing. I’m going to start as usual, I’m Dr. Gail Newel, health officer of the County of Santa Cruz. I’m going to start with the usual briefing of our data points. And I do want to tell you that as of last night, we launched our new data dashboard.
And I think you’ll find it very physically appealing, and also has much more data, the kind of data that the community has been asking for, but we just didn’t have enough cases yet to break things down in a way that would protect patient privacy. And now that we have more cases, we can do that. So, I’m going to use our data dashboard data and report out to you on some of that. So at this time, we have 76 known cases of COVID-19. That was on the data dashboard last night.
OK, so data dashboards found at santacruzhealth.org. And so as of this morning, I guess it was updated since 5 p.m. last night, we had 80 known cases, with still just one death of a Santa Cruz County resident.
The breakdown of those by age is: two in the pediatric range, so under 18, 14 who are 18 to 34, 28 who are 35 to 49, 20 who are 50 to 64 years old, and 15 over the age of 65. One of the cases is still under investigation to determine age. Of the known cases, the 80: 35 are male and 45 or female.
We’ve been able to break down the type of exposure for some of the cases. 20 of the cases remain under investigation, but the remaining 60 are broken down as follows: 12 of our cases are travel related. So we knew from early on that we had some cases from the diamond Princess and the Grand Princess and we’re also expecting to get some travelers from the two ships who have boarded in Florida.
Twenty-five of our cases are community acquired, which means there’s no specific source located, so they were acquired somewhere in the normal day to day business of folks moving around the community. And 23 were acquired through a close contact. So a known positive case with contact to these folks.
Of the 80 known cases, 13 required hospitalization during their COVID-19 illness and one of those died. 30 have recovered. That’s a new number that we’re just releasing now. And we’ve firmed up our definition of “recovered” working along with the California Department of Public Health to define what “recovered” means. And 30 of our 80 have recovered. So that’s fantastic news.
In terms of the number of cases tested or the number of labs performed, we know our positives, so the 80 cases there. In addition, we’ve had a number of additional cases tested through the public health lab, with the remainder being through commercial labs like Quest and LabCorp. And so our negative lab test results we’ve had are close to 1,500. So 1,469.
This is nearly a doubling of our negative lab test results in just a week. So we see that testing is finally ramping up. There are at least three healthcare systems who plan to have testing next week. So that’s very exciting. One being Dominican Hospital, another being that Dignity Health Systems, and then also here on our own Emeline campus in our clinic located here.
Our known cases by geographic area: 27 of the cases are in North County, 30 in Mid County and 14 in South County, nine are still under investigation to determine location. We do have breakdown by city and by area census tract and that sort of thing. But the numbers are too small to release at this point and still maintain privacy. But what I can tell you is everywhere has known cases.
And when I say known, we’re assuming that there’s a greater number by far of unknown cases, some folks have estimated some experts have estimated possibly as many as 20 unknown cases for as, as far as, and in addition to the known. For each known, 20 additional unknown cases. That’s a very loose estimate, however.
I’ve already talked to you about the new dashboard, data dashboard on our website.
Let’s see what else is on the dashboard that I haven’t covered. The dashboard also covers chronic conditions, disease conditions in known cases. So it’s broken down by one or two chronic disease conditions.
So you can see that and as expected, those with hospitalization were more likely to have underlying chronic disease conditions, also more likely to be male and more likely to be older. We also have graphs demonstrating both are known cases, new cases by day. And in addition, our cumulative counts and also broken down by geographic region.
As I mentioned, there’s also on our website, a new graph posted that shows the curve or doubling time of Santa Cruz County compared to all of the other counties in the state of California. And there’s very optimistic news there, although it’s also very early, but we are among the very best counties in the state of California in terms of flattening the curve. So instead of a doubling time, every six days, as we had anticipated would happen in a community like ours, we are now having a doubling time of eight days.
A two day difference doesn’t sound like very much, but it’s huge. And so I want to make sure that the community understands that this is because of them and their efforts and their willingness to shelter in place. So I want to thank our community members for following the social distance requirements and sheltering in place.
Hard news, I think the community mostly knows that I’ve issued a supplemental health officer order to close all of the beaches and all of the parks in our county for one week. And the reason we did this was In anticipation of this holiday weekend, we expect the weather to be better, to be sunnier.
Traditionally, many people celebrate Easter outdoors. Many religious groups gather during this time. Passover is also happening now. And so we want to make sure that the community understands that gatherings of any size are not allowed, even in outdoor spaces.
And we want to discourage people from using our parks and our beaches to gather because this is where infection rates are shooting up, where we’re seeing big death rates and, and infectious outbreaks is when people gather in large groups, whether it be for funerals, for church services, for social gatherings.
So it’s so important that our community understands that that is not allowed by the current health officer orders and from an infectious disease point of view is very dangerous.
So I think I’ll end there for now. Would either of you like to add anything in terms of a statement?

DR. DAVID GHILARDUCCI: I could talk a little bit about our PPE [personal protective equipment] distribution. Yeah, I’m Dr. David Ghilarducci. So, there have been a lot of requests from the public and from our healthcare providers for PPE as you know there’s a nationwide shortage.
There’s some encouraging news at the state level that they’ve been able to acquire, I think up to 20 million masks a month now that should be distributed and we’re, we have a system in place where we request those resources to come.
We’ve also prioritized what types of PPE go to whom and have allocated it based on the sort of size of the organization and the type of medical activity that they perform.
We are looking at even non-medical kind of congregate settings like assisted living and board and care and getting some protective equipment to them as well, that’s appropriate for that setting.
And then, of course, an important aspect are facial coverings for the public. And that’s been handled through a separate division through donations. But that is part of our PPE, if you will, distribution. So that’s all I have for that.
MIMI HALL: Yeah, I think I can talk a little bit about alternate care sites. Many of you know that we’ve identified two alternate care sites: one at Simpkins Swim Center, and another one at 1440 Multiversity.
And it’s important to know that how and when we implement these sites is related to the data that we have and the number of cases that we have. So as we flatten the curve, our projections for when we will implement or activate these alternate care sites also extends, so we had originally had a request in to the state for disaster service and Medical Reserve Corps workers to start on Monday.
But our hospitals are not seeing the surge as early as we had thought three weeks ago due to the increased doubling time. So we’ve delayed that request for a couple of weeks. And if our community does really, really well, with social distancing, we hope we can delay that even more, perhaps indefinitely.
One of the things I do want to note is that when we are ready to post our modeling curves for projections, they will be refined every week based on actual data. And there is a best case scenario and a worst case scenario. We prepare for the worst case scenario. And there is a worst case scenario that has us exceeding the number of beds available even with our alternate care sites.
And so, one of the things that the state has been really active in doing the last couple of weeks is taking a look at California regionally. So we were actually contacted by Seton Medical Center. It’s a facility that the state bought to be a federal medical station. And they have said that they will be receiving patients from Santa Cruz should we experience surge that exceeds our hospital system in our alternate care sites.

REPORTER: Yesterday, Jim Hart was talking about how he supported possibly extending the order of the closures of beaches and parks. And I’m wondering at this point, what is the likelihood that you’re going to do that given the summer months are coming, coming up?
DR. GAIL NEWEL: I very much valued the outdoor spaces that we have in our community. And I know that all of us do, and it’s a big reason why we live here, the outdoor beauty. And most of us rely on the beaches and parks for not only our physical health, but our mental health as well.
There’s also an issue of equity, that the poorer you are, the harder it is for you to get to an outdoor space. For example, we know in the South County there’s far less park space per capita than there is in the north part of our county.
And for those reasons, my intention is to reopen all of the parks and the beaches in one week, the order, the supplemental order is for only one week. It may be that there are areas, specific parts of parks that I do not reopen.
For example, despite our warnings the skate parks have continued to be a problem and social distancing has not been able to be maintained in the skate parks. Same in the dog parks.
So it’s likely that I will extend the closure of the skate parks and dog parks. But I do intend to open the rest of the outdoor spaces at the end of the supplemental order next Wednesday at midnight.
JASON HOPPIN (COUNTY SPOKESMAN): Nick, go ahead.
NICHOLAS IBARRA (SENTINEL): I’m wondering if you can talk a little bit more about the growth curve that we’re seeing doubling every eight days. And it looks promising on its surface. But can you explain how residents should be looking at that? And any challenges with interpreting too much into that curve? Whether that relates to testing or anything else? How should we be looking at that rate at this point?
GAIL NEWEL: You’re exactly right, with only 80 known cases any modeling we do for our community is very tentative. And we’re really looking at it on a day-to-day basis. And if you are able to look at the model on the data dashboard that’s released by the state, you’ll see that our curve is much flatter than the rest of the counties.
That’s due to, I believe, to our community’s excellent response to sheltering in place. So that’s what’s working, where you’re not ready to lift that now.
And as you see with my beach and parks closure, I’m especially worried about continued compliance with those orders. So, was there another part to your question I may have forgotten?
NICHOLAS IBARRA: Yes. Just, is there anything that you’re aware of particular to Santa Cruz County that could be influencing that data, such as testing numbers, or any other area beyond social distancing working? Is there anything else here that could be artificially lowering those numbers compared to some of these other counties? Or as your sense that, at least based on what we know, social distance seems really has worked here better than in some other areas.
GAIL NEWEL: Right, well, in addition to known cases, we also look at hospitalizations and ICU admissions. And those can be used as a proxy for known cases and spread in our community and those jive very well with our number of cases.
So everything points that we’re moving in the right direction, and that the community members really need to continue to do what they’re doing because it’s working.
KARA MEYBERG GUZMAN: What’s the latest number of hospitalizations and number of ICU beds occupied? Is it possible to get that number more frequently updated on the data dashboard? And third, is it, are we testing everyone who’s an inpatient?
GAIL NEWEL: There’s a new website that they California Department of Public Health that is updated daily with data. The hospitals are now required to report to the state every single day with their current bed count and their current bed capacity. And so, you can go to that state website and you can click on Santa Cruz County, and you can see our current bed count and capacity, as well as the current number of COVID cases who are hospitalized in our county. And that’s updated every single day.
PHIL GOMEZ (KSBW): Are you concerned that people are, you know, with all this good news and everything else that people are going to drop their guard and perhaps, you know, disregard some of the social distancing and the like, I mean, it appears to be working. But you know, all this good news may lead people to, you know, forget these these rules and, and meet in groups and the like and all it will take is one to make this grow even bigger again.
GAIL NEWEL: You said it exactly right, Phil, I couldn’t have said it better. I am concerned and I’m concerned as we get sunnier weather and warmer weather. And as summer approaches, we’re going to have more travelers come to our area. There’s measures that we’re taking.
I’d like to commend the sheriff for his invaluable partnership and our local law enforcement. We’re also working very hard at working with the Airbnb, VRBO’s and hotel industry to make sure that they’re only housing essential travelers, so people who are here to do essential work only.
We do not want vacationers in Santa Cruz County at this point, because they will bring the virus from their more infected communities, especially if they’re coming from San Francisco, San Mateo, Santa Clara, our neighboring counties who are experiencing much worse impact from this virus then are we.
DREW ANDRE (KION): Now that there is a recovery number and we have some of those cases recorded, what is the follow up with those patients as far as public health goes, and then if this is available, do we have a broad age range of those people who have recovered?
GAIL NEWEL: As I said, most of the ones who have been hospitalized and the one who died were older age, mostly male, mostly with an underlying chronic medical condition. So you can assume that the recovered ones are opposite of that they’re healthier, younger, more often female, more resilient overall with, in better physical health. Our infectious disease unit, communicable disease unit, to this point has been able to follow each individual case and notify each of their household contacts, their close contacts, employers, schools, entities in which they may have had close contact and work to identify further cases.
That’s how we’ve identified, I think it’s 23 of our cases. Yes, the close contact cases. And so, at this point, our numbers have not been overwhelming. And so we’ve been able to do that.
KARA MEYBERG GUZMAN: Just follow up on my last question, is every single person who’s hospitalized, like every single inpatient, are they all being tested for COVID? And also, a question about PPEs: Is every single hospital employee receiving PPEs or just the ones in contact with people suspected of COVID?
DAVID GHILARDUCCI: Want me to take both? Yeah, as far as who gets tested in the hospital, our understanding is that most hospitalized patients are being tested if they’re considered to have symptoms consistent with, you know, a viral infection.
KMG: You have to have symptoms?
DAVID GHILADRUCCI: Typically, now this is going to be some variability depending on the clinician that’s taken care of the patient. But I, but we’ve certainly prioritized testing toward that population, because it’s important for the hospital personnel to know because it helps with not necessarily treatment but also disposition and, and PPE preservation and so forth.
So that is a prioritized group, they have an expedited testing process typically return, the turnaround times for those folks are about 24 hours, whereas it had been much longer for everybody else.
We’ve also prioritized testing of health care workers. I want to emphasize though, that testing does not work when you’re asymptomatic, or at least, the reliability is very low.
So there’s a consequence of getting a test when you don’t have symptoms, that you get a false negative, you get a negative result, that may actually not be the case. And so you have this false assurance that you’re somehow fine and free of virus when in fact may actually be infectious and, and so, so we don’t, or we really caution against testing of “well” people, but there’s a lot of anxiety, of course.
Now the second question, the PPE: does everybody in the hospital wear PPE? The hospitals have been responsible for their own policies, and my understanding is both hospitals: Watsonville, Dominican and also Sutter have ㅡ I believe Sutter has ㅡ have implemented a universal masking or facial covering policy.
So even people that are working in administration or are like in registration and so forth, that may not have direct patient contact, they’re wearing some form of facial covering. It’s really important right now until the supplies of PPE come up, it’s important that we don’t divert, you know, the real PPE if you will, the medical-grade PPE to people who aren’t in a medical setting, so, so it’s a kind of a tiered approach there.
MIMI HALL: One of the things I’d like to mention about our PPE distribution is the Centers for Disease Control and Prevention does have guidance on use of PPE and optimizing it when we have shortages. So right now we’re in something called contingency status.
If we have even fewer, we’re going to move to something called crisis status. And so when we distribute our future PPE we’re asking that all of the requesters in the healthcare system give evidence that their, their burn rate and their strategies are optimizing PPE right now, according to contingency status.
STEPHEN BAXTER: Can you, can you talk about the long-term plan to get everyone out of lockdown, since things seem to be going better than we thought?
GAIL NEWEL: Say it one more time? Lifting the lockdown?
STEPHEN BAXTER: This is Stephen Baxter with Santa Cruz Local. Since things seem to be going better than anticipated, what’s the plan for lifting the long, long-term lifting the lockdown?
GAIL NEWEL: Well, it’s not really a lockdown because a lockdown would be that people cannot legally come and go from our county and it’s still possible for people to come and go from the county as you know. So the order is a legal order but it still allows lots of movement for our residents. So not truly a lockdown. So I want to avoid using that term.
It’s gonna be a while until we lift the shelter in place. As you know, the current shelter-in-place order extends into May. And we are anticipating that that probably will be extended as our current modeling shows that’s going to be about the time that we have a surge in healthcare needs. That’s not going to be a good time to lift or shelter-in-place order. That’s when our cases may be at their peak or at least the shoulder. And if things go as anticipated, the shelter in place will be extended.
DAVID GHILARDUCCI: If I could add just, excuse me, I was using this earlier with Mimi, I was, I used to be a firefighter before medical school. And this is very similar to that kind of scenario where, you know, you go into a fire you do the knockdown phase, you got the flames out, there’s smoldering embers, here and there. And if you then packed up your hoses and left, and left everything to where it was, it’s going to rekindle.
And so the, the, the issue is very similar in this situation that we’re in the knockdown phase right now, with the social distancing the shelter-at-home orders, the closure of the beaches. It’s very important that we don’t, that we don’t relax some of these restrictions too soon, because you will get that rekindling. So if that’s a helpful way of thinking about how this works, I think it’s relatively straightforward. Thank you.
STEPHEN BAXTER: What, two questions: one, what data point will you look for in terms of lifting Shelter in Place? I know you talked about hospitalization. On April 1, it was it was nine, now, yesterday was 14, Today it’s 13. Obviously, we have a ways to go but is that the key stat? Like what, what should we be looking for?
GAIL NEWEL: Um, because our testing is not widespread we are relying on hospitalization and ICU admissions for ㅡ to give us a better idea of where we’re going with the infection in our community. Obviously, if we had larger numbers, hospitalized and in the ICU, we would be really concerned that we’re missing a lot of cases in our community.
But as I mentioned earlier, the hospitalization and ICU numbers indicate that we’re capturing a fair number, enough of a number in our outpatients to know where we’re headed.
MIMI HALL: And this is Mimi Hall. I’d like to add Dr. Ghilarducci’s example of putting out a fire but then embers starting a hotspot. That’s when the testing ㅡ expanded testing capacity is really going to be a useful tool is, as we get control of this, when we start having new cases in different places, the testing is going to be the thing that allows us to understand where that’s happening and properly control new small outbreaks in regionalized areas.
And we’re getting there. And there’s going to be massive expansion of testing capacity in the next few weeks.
DREW ANDRE (KION): Following up on the testing, could you elaborate on the, the three new testing sites that you mentioned?
GAIL NEWEL: There, I know that Dominican Hospital has acquired a system to do point of care testing. So the test is performed right there at the hospital. Their intention is to initially use it only for their own patients in the hospital. So whether it’s inpatient, or people who were in the emergency department, they’re not going to run it on mild cases or people who just want to know, it will be used for “hospital sick” level patients. They’re hoping to be ready to run with that next week.
I know there are nationwide shortages of both reagent and swabs. So it’s not enough just to have the equipment. And then there’s a training component as well and a quality assurance component. So I don’t want to promise on their behalf that the testing will be available, but they’re hoping for next week.
Same with Dignity. Dignity has another point-of-care system with an even more rapid turnaround time than the Dominican Hospital. And my understanding is that they already have the reagents and the swabs in place.
And that, I believe they’ve got four pieces of equipment, so they may be doing it at more than one site.
And then the third is our own clinic here on the Emeline campus and also point of care testing. So the tests are performed right here in the county, right here on site.
MIMI HALL: I would like to add a reminder that these aren’t public testing, so people should come to the drive thru clinics and they still need a referral from their provider, no matter where they go.
KARA MEYBERG GUZMAN: Kara Meyberg Guzman from Santa Cruz Local. Because it sounds like, from what you’re saying, Santa Cruz County is doing a little bit better than the, doing better than other counties in the state. Would you ever consider, you know, maybe limiting entry and exit from Santa Cruz County setting up checkpoints?
GAIL NEWEL: That is a possibility. Two of my fellow health officer colleagues did that this past week. So both are in the Sierra area, one in Mono County and one in El Dorado County.
In both of those counties there’s very limited hospital capacity and health care capacity, but large numbers of vacation homes. So what they were seeing was families from Sacramento, San Francisco, Santa Clara with a ski condo for example, or home up in the Sierras, were spending their shelter in place time in their vacation home. And then those folks would fall ill and, having been exposed in their home communities, bring it into Mono or El Dorado County and place a burden on the health care system that they were not ready to handle.
I know there was a case in Mono County of someone who needed to be helicoptered out because they were critically ill. But because of the snowy conditions, the helicopter took almost all day, which really delayed the care of that critically ill patient.
And so we encourage people to shelter in place at their primary point of residence and not utilize their vacation homes for this time.
SOMEONE: We have another question on the phone.
NICHOLAS IBARRA: This is Nick Ibarra with the Sentinel. Can, let me just ask this really quick and then then go ahead. So my question is related to the long-term and short-term projections that you mentioned earlier. Sorry, the best-case and worst-case projection. What can you tell us about each of those cases, the best case scenario and worst case scenario and why not release those projections to the public at this point to better inform people about the data that is informing your decisions?
GAIL NEWEL: I think we’re getting there, I think we’ll be releasing those projections very shortly. We’ve already presented them to our board of supervisors in a closed session, and to some of our healthcare partners as well, and to our own Emergency Operations Center.
That as our numbers grow, we’re more confident about our projections. It’s sometimes difficult for the community to understand, and they get very worried about the worst case scenario. And so we’re trying to balance the fear factor per se, that these might present if folks are focused on the worst case scenario.
And also there’s other people as has been mentioned, already, if they look at the best-case scenario, they might feel really good about getting out of their house and, and not following shelter in place. So it’s more about how can we make these more interpretable to the public and make that information best understandable.
DAVID GHILARDUCCI: It might excuse our mid Dr. Ghilarducci here, because the, the numbers that are fed into the model are so small, that the, the, the usefulness of these models, they could change from week to week. So, it in some ways may not add a lot of information for your readers if, if we release models that don’t have some degree of certainty to them.
GAIL NEWEL: And they may, if they’re changing week to week, they may undermine the trust of the public, if it’s a constantly changing target, right? So we’re trying to be judicious about what, how useful the information is.
ASHLEIGH PAPP: Thanks again for doing this. This is great. Um, I’m curious to hear more about our at-risk communities. So the homeless groups and migrant communities. How are they faring right now? And are there any kind of targeted preventative actions that you guys are working on?
GAIL NEWEL: I’m so glad you asked because I was going to bring it up if you didn’t. Our communicable disease unit is shifting its focus now from individual cases, to working with congregate living settings. So of course, our most vulnerable population who lives close together in groups is our persons experiencing homelessness. And we’ve partnered with the Human Services Department to ensure that more and more of those folks are sheltered every day.
So as you probably heard, the vets halls have opened for sheltering purposes in both Watsonville and Santa Cruz. And in addition, we are beginning to hotel people and motel, in the Beach Flats area of Santa Cruz and we have additional contracting going on with more motels and hotels.
We’re planning to provide isolation housing for people who have COVID-19 and need to be separated out from the community, but don’t have their own home to do that in. So the hotels and motels will be helping to do that. And same with quarantining or, their close contacts. And then right now, we’re also housing some of the elder homeless individuals as well as those who are medically fragile.
Our other efforts are focusing on skilled nursing facilities. You’ve probably seen in the media that these have been hot points for other communities who are in the middle of their surge, even in Southern California, some of them having to be evacuated because staff have not been able to come to work for lack of personal protective equipment. So we’re focusing our efforts now working actively and proactively with the skilled nursing facilities to ensure that they’re able to receive COVID positive patients, and learning how to protect and cohort house those.
In addition, we’re very, we’re working very closely with the jails. And again, I want to thank Sheriff Hart for his cooperation and collaboration in doing this. The jails have been doing screening and readying themselves already for two months. So they’ve been very proactive, we’ve been working closely with them, and then any other congregate living settings such as residential care facilities, long term care facilities. We’re working proactively with all of those to get them ready for COVID patients.
DREW ANDRE (KION): Dr. Ghilarducci, last week, you mentioned that the rough projection of when ICU bed spaces would fill up is end of April or early May. Has that changed at all this week?
DAVID GHILARDUCCI: No, looks the same. In fact, there are early indications that it may be long ㅡ later than that, but we’re still using those numbers, those dates.
KARA MEYBERG GUZMAN: For Dr. Ghilarducci. You said last week that it’s not a matter of if but when we exceed our surge capacity ㅡ is our max surge capacity of ICU beds still 50 beds? And what’s the plan for when ㅡ if and when we get there?
DAVID GHILARDUCCI: When we exceed that, OK. Well, the some of the sort of fallback positions are requesting more ventilators from, from the state if those are available, we’re hoping that maybe as other places that are hotspots like New York state, maybe in the next couple of weeks, they’re able to release some of the ventilators that they have and those can be moved to others ㅡ where new hotspots come. So getting those will be important.
It’s not just a matter of having the machines and I think I said this last week, we need the people to know how to, how to manage a ventilated patient and, and that is a physician skill that not everybody has. But there are a fair group of people like anesthesiologists, emergency medicine people that wouldn’t traditionally manage people events, but have, you know, the sort of training experience to do that.
So, so I hope we don’t get to that number, we’re preparing for getting over that capacity. And what you’ll see, though part of the intent of the alternate care side is that the cohort of patients that are in the hospital will get sicker and sicker, and we’re going to try to relieve the strain on the hospitals by taking those patients that are kind of in transition from being in the hospital and going home and then providing a kind of transitional sort of place to be until they get well enough to go home. So we’re hoping that, you know, essentially, those spaces will open up for sicker people, but –
KARA MEYBERG GUZMAN: And is it still 50 beds, is that their max surge capacity?
DAVID GHILARDUCCI: Yeah, the number can vary a little bit. I’ve been kind of using 49, but it depends on, there’s a lot of little details in there about what kinds of events and whether ㅡ they’re pulling some out of storage and refurbishing. So I would say roughly 40 to 50 would be something I would count on.
STEPHEN BAXTER: Given that Santa Clara County has done more than 11,000 tests and our county has done about 1,500, how useful is it to compare number of cases county to county?
GAIL NEWEL: Santa Clara is, we believe, two to three weeks ahead of us on the curve. So I don’t think it’s just a matter of the number of things test done per capita, per capita, but also the ㅡ an indication of the prevalence of disease. They have more sick people there and people who are sicker, far more hospitalizations and death than we have. We hope we never get there ourselves even on a per capita basis. But at this point, they ㅡ we do look to them as part of what lessons that we can learn.
MIMI HALL: And this is Mimi Hall, I will point out that Santa Clara’s doubling time, which is an important number to look at is much shorter than our counts. So that means that there, the spread is faster there.
MIMI HALL: Actually, the state ㅡ the dashboard that Dr. Newel mentioned earlier, where you can go to the state and see every day in real time hospitalization. The state’s also taken over collecting daily statewide, other kinds of more detailed information from the hospitals and so what they’re trying to do is assist the locals.
So if we get to a surge in one of our hospitals, and they’re seeing that we’re nearing capacity, they have the ability to quickly in a day, take a look at what regional hospitals have room so that we can work within our regional systems to get patients to the care that they need.
GAIL NEWEL: So that’s a follow up to what Dr. Ghilarducci mentioned about the 50 ventilator capacity. In addition to the 50 we have Seton on standby for us. And then this morning I was on a healthcare leadership call, where the leaders of Kaiser Permanente pledged to include Kaiser in their regional approach to ICU and ventilator beds. That was very good news.
JASON HOPPIN: Thank you, everyone. We’ll do this again. Next week, if not sooner.
REPORTERS: Thank you, thank you. Thank you very much.
GAIL NEWEL: Have a good weekend even without your beaches and parks. Thank you. You too.
KMG: If you’re on our email newsletter, respond to our email with your questions for our public health officials. We’ll ask your questions at next week’s press conference.
You can sign up for our free email newsletter at santacruzlocal dot org.
[MUSIC]
Thank you to all our members. We can’t do this without you. Thank you especially to our guardian level members: Chris Neklason, Patrick Reilly, Elizabeth and David Doolin, and the Kelley Family.
If you find our work valuable, become a member. Membership sign up is at santacruzlocal.org/membership.
Thank you to Natalya Dreszer for the transcript of this episode. You can read it at santacruzlocal.org.
Thanks to Trimpot for the music.
I’m Kara Meyberg Guzman
SB: I’m Stephen Baxter.
KMG: Thanks for listening to Santa Cruz Local.
Kara Meyberg Guzman is the CEO and co-founder of Santa Cruz Local. Prior to Santa Cruz Local, she served as the Santa Cruz Sentinel’s managing editor. She has a biology degree from Stanford University and lives in Santa Cruz.
Stephen Baxter is a co-founder and editor of Santa Cruz Local. He covers Santa Cruz County government.






