Details emerged this week from California and Santa Cruz County leaders on what it will take to lift the shelter orders. The county still lacks about 50 ventilators it needs for a potential peak of 100 severe COVID-19 cases, county health leaders said. That peak could come as late as June. Santa Cruz summer traditions remain up in the air, including the Wharf to Wharf footrace, Junior Lifeguards and visits to the Santa Cruz Beach Boardwalk.
EPISODE TRANSCRIPT
Transcripts are usually only available to Santa Cruz Local members. We offer coronavirus-related transcripts free as a public service.
To read the transcript for Thursday’s news conference hosted by the county health services agency, click here.
KARA MEYBERG GUZMAN: Hi everyone, Kara Meyberg Guzman here. I wanted to give you a behind-the-scenes look into what goes into Santa Cruz Local. This week alone, Santa Cruz Local attended or watched online: the Santa Cruz County board of supervisors meeting, the Santa Cruz City Council meeting, news conferences hosted by the governor and the Santa Cruz County Health Services Agency, a talk by UC President Janet Napolitano and two telephone town halls hosted by two county supervisors. We report to you what you need to know.
And, today, Friday April 17, we’re hosting our own livestream town hall. It’s at 12:30. We’re hosting Dr. David Ghilarducci. He’s the county’s deputy health officer. And another special guest, Dr. Larry DeGhetaldi. He’s the Sutter Health Palo Alto Medical Foundation Santa Cruz division president. They’ll answer your questions on the coronavirus. It’s free. You don’t need to be a Santa Cruz Local member. The registration link is in our show notes.
But become a member. Last year, about 80% of our revenue came from memberships from people like you.
Sign up to support local journalism at santacruzlocal.org/membership.
[THEME MUSIC]
STEPHEN BAXTER: I’m Stephen Baxter.
KMG: And I’m Kara Meyberg Guzman.
SB: This is Santa Cruz Local.
This week, Santa Cruz County leaders and Gov. Gavin Newsom shared details on what exactly it will take for us to get out of the shelter-in-place orders.
On Tuesday at the board of supervisors meeting, Santa Cruz County Health Officer Dr. Gail Newel said she expects a looser shelter order for May 4th. It will replace our current order. She basically said it has to be aligned with other Bay Area counties. She also said that county orders can be stricter than the state but they can’t be looser than the state’s guidelines.
Ultimately, it’s up to the governor to set the baseline.
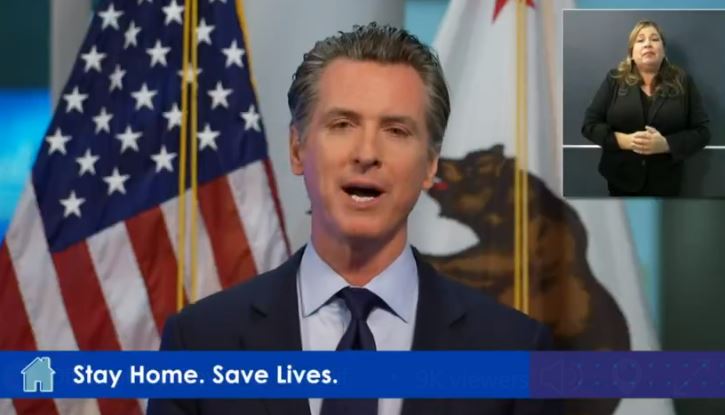
This week, the governor gave the most detail yet on the criteria for easing the shelter order.
Six factors go into it.
- Testing. Does the state have enough tests and staff to monitor the spread of COVID-19?
- Are vulnerable groups such as senior citizens and people in jail, supported enough to physically distance?
- Can hospitals handle surges in patients? Do hospitals have enough beds, staff and supplies?
- Do people have access to healthcare to recover outside a hospital?
- Can businesses, schools and childcare centers support physical distancing?
- And finally, can modified shelter orders be communicated quickly?
Newsom recognized that businesses and workers are suffering from the shelter order. It’s expected to be loosened in the coming weeks. But he said it’s not like a light switch. It doesn’t turn on and off. It’s more like a dimmer. He said shelter orders could be loosened and tightened depending on conditions.
He said the state’s working with school leaders to deal with distancing. Also, restaurants could open, but they might look different. Here’s Gavin Newsom.
GOV. GAVIN NEWSOM: We talked about what the new normal will look like. As I said, normal, it will not be. At least until we have herd immunity and we have a vaccine.
Because as someone like yourself that looks forward to going back out and having dinner, as the doctor said, you may be having dinner with a waiter wearing gloves, maybe a face mask. Dinner where the menu is disposable. Where the tables, half of the tables in that restaurant no longer appear. Where your temperature is checked before you walk in to the establishment.
These are likely scenarios as we begin to process the next phase, the next iteration. For businesses, the same opportunity and responsibility resides to allow for their employees to practice a safe physical distancing.
KMG: At the board of supervisors meeting on Tuesday, we heard about the local criteria for easing the county’s shelter-in-place order. Health Services Agency Director Mimi Hall shared her four criteria.
- Tests for every person with symptoms.
- A 30-day supply of protective equipment like masks and gowns for health care workers. They’re a long way from that, she said.
- Declining cases and deaths for two weeks. This hasn’t happened yet.
- More county epidemiologists to trace cases. They just hired two, for a total of seven.
On Thursday, I attended a news conference at the county health services agency’s Emeline clinic in Santa Cruz.
I asked Director Hall for the status of three of those areas: Testing, protective equipment, and people power needed to trace cases.
As of Thursday, we had 98 confirmed cases and two COVID deaths in our county. Remember that the county doesn’t have enought testing to even test all the people who have symptoms. So that’s not really an accurate signal of how far the virus has spread. County leaders keep saying that they’re ramping up testing. But cumulative COVID tests in our county as of Thursday was about 2,500. A week before that, it was about 1,500 tests.
Here’s Director Hall on testing. You’ll hear some dings in the tape. That’s reporters calling in on the conference call.
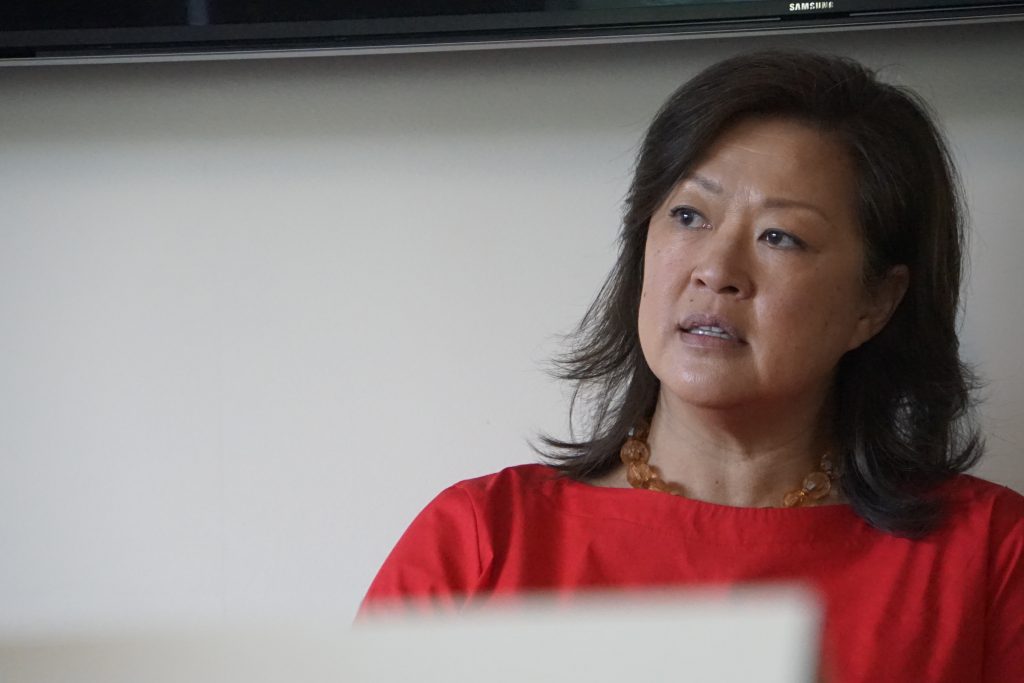
MIMI HALL: So in terms of more testing, we actually are ramping up our testing capacity. We have our commercial labs who have really shortened the length of time that they are responding back with test results. Some of the commercial labs a couple of weeks ago, were getting us results seven to eight days later. And now it’s more like two days, four days. So that’s a positive.
The other positive is that we do have local testing available now through a few sites and one of those sites is our own county clinic. It’s important for people to know that those testing sites are for patients of those areas.
I think that in the long term, there’s some thinking that we can do. And we’ve already started that thinking about how we can make the shift to community-wide testing. We’re not there yet. But we don’t need to be there yet. We have to be ready for that place, maybe in a couple of months, and we start coming down the curve and thinking about how we’re going to further lift shelter in place. But that’s phased in.
In terms of workforce, that’s another thing that we’ve been thinking about. Just as of two weeks ago, we’re planning on workforce for alternate care sites. And we’re still on that plane. Now, we have to start planning for our workforce in three to six weeks from now and beyond. Because, again, if there is going to be any shift in the disease, perhaps related to any changes to shelter in place, we’re going to have to have the workforce and there is a robust system. A lot of different counties are actually starting to make plans for that. And we’re — we’re doing the same. What were the other things?
KARA MEYBERG GUZMAN: PPE?
MIMI HALL: PPE. Yeah, so PPE. There’s a little bit of good news. It’s not great news, but we do have – we’re receiving, it seems to be like weekly shipments from the state. And I hope that they continue and it’s not everything that we asked for, but they’re enough to get us by.
We are still in something called contingency status. So the CDC for PPE has three statuses. One is conventional, meaning you operate as normal, you follow all of the safety precautions you normally would. But then when scarcity begins, there’s contingency and crisis status. And so we are right now as a nation in crisis — or in contingency status. So that means that we really have to preserve PPE across all different kinds of workers and we’re really encouraging the public and people who aren’t direct medical care service providers to not use medical-grade PPE.
One of the things that Dr. Newel has mentioned is – so what about the downside of the curve and having enough, your question of broad testing, testing requires PPE. So to even get to that place where we think that we could, we have to get out of contingency status. And getting out of contingency status means that we’re going to as a community have about a month’s worth of PPE stock on hand for the healthcare system.
KARA MEYBERG GUZMAN: Are any of those the limiting factor in terms of when we can start lifting some of the shelter in place?
MIMI HALL: No, I think the limiting factor is really — the biggest limiting factor is disease. We have got to see our cases and our hospitalizations start decreasing. So for those of you who think if we just get you all PPE, if we just get you testing, I mean, that’s only part of the formula. We actually have to see the cases start decreasing.
KARA MEYBERG GUZMAN: And then I asked her how many more epidemiologists are needed to trace cases.
MIMI HALL: Well, I mean, that’s just such a loaded question. It’s kind of like how much money do you need? I feel like we have great capacity with our epidemiologist right now. And they have good partnerships with colleagues in other institutions as well. So I think that we need person power in a lot of different areas. We’re able to keep up with the tracking and the modeling and the data input.
Some other areas it’d be really great to have staff is, so when we move away from where we are, and we’re going to look at this long-term mitigation it would be really great to have people who are great at data. And by data, I mean, data embedded in health information exchange, to pull surveillance information, symptomatic information, data to the public so that we can use apps on our phones so people can self report. So those are all the things that would be really great for us to build the capacity to do.
SB: As of Wednesday, Santa Cruz County had 11 people in the hospital who were COVID-positive or suspected COVID-positive. Five of them were in intensive care. That’s according to the hospitals, who report to the state.
Dr. Ghilarducci, the deputy county health officer, said the thing he’s most worried about is the intensive care unit capacity.
DAVID GHILARDUCCI: Currently, we think we have about 400 hospital bed capacity in the county that’s combined of three inpatient facilities. That number may vary a little bit depending on certain conditions. We have about maybe 45 to 49, ICU or ventilator capacity beds. The projections are that state projections at least released recently suggests that Santa Cruz may experience – most likely experience about 300 hospitalizations at peak.
So bed supply of 400 — 300 at peak — we should be OK there if it goes as, as is most likely. Obviously, these are broad curves and there are many possibilities.
I’m a little more concerned about ICU capacity. And I’ve mentioned that before here. They’re projecting that we may need up to 100 ICU or ventilator beds at time of peak. And as I said, we have less than half of that. So we’re working very hard to find ways to expand capacity and that would include moving patients to where — to other counties where ventilators may be and so a very fluid situation.
KARA MEYBERG GUZMAN: Well, is that, that regional help — is that enough to meet those 50 extras?
DAVID GHILARDUCCI: Yeah. That’s a great question. Now in a normal time, you know, we can, we can safely rely on outside hospitals to provide extra help. During this pandemic, we are not assuming that that will be available. So, we have to look for internal resiliency to the extent that we can.
And so that’s going to probably mean some real creative solutions. You know, getting ventilators from the state or the feds would be helpful, finding people to staff those ventilators, the medical professionals that you need to provide that intensive care.
There’s other things that ICU patients need besides just the ventilator itself. There’s lots of medications that, they could have six or seven medications, infusing at one time for very, very sick people. So lots of labor involved there. And so the people part of it will be important as well.
SB: One last takeaway from the county health officials this week. Summer in Santa Cruz may look a bit different this year.
Dr. Newel said Thursday that she does not anticipate legalizing gatherings of any size for a long time.
That means that registration for Wharf to Wharf race is already on hold. And the Santa Cruz Beach Boardwalk may or may not open all summer.
Newel did say that summer day camps for kids are possible and they’re working on how to do them. And also the Junior Lifeguards program may be possible but it could look different.
In terms of COVID cases, the peak was originally projected to be this week. Now, it’s pushed out to mid-May or early June, according to county health leaders.

GAIL NEWEL: This is going to be a slow, long process. And restrictions are going to be — need to be lifted very carefully and slowly a bit at a time. And then restrictions may have to be placed back depending what we see on the disease, disease curve.
So we really think that instead of one big curve, we’re going to see a series of ripples. So I’ve been saying, you know, instead of a tsunami, we’re going to have a series of ripples and asking Santa Cruz to ride the waves.
[MUSIC]
SB: If you’d like to know what else was said in Thursday’s news conference, we posted the transcript on our website. We’ll put the link in our show notes.
And a reminder, we have our Santa Cruz Local Town Hall, today, Friday April 17, from 12:30 to 1:30pm. Our guests are Dr. David Ghilarducci and Dr. Larry DeGhetaldi. The link to register is also in our show notes.
KMG: By the way, we’re having a special members-only event over Zoom on Tuesday. We’ll discuss how we can help our community get through this time. Members, your invite will be in your email in the next few days.
If you’re not a Santa Cruz Local member yet, it’s not too late to sign up.We’re trying to reach 600 members by the end of the month. As of Thursday, we’re at 341. Sign up is at santacruzlocal.org/membership.
SB: Thank you to all our members! Thank you especially to our 16 new members who signed up this week. And as always, thank you to our guardian level members: Chris Neklason, Patrick Reilly, Elizabeth and David Doolin, and the Kelley family.
Thanks to Trimpot for the music.
Special thanks to Natalya Dreszer for the transcript of the news conference.
I’m Stephen Baxter.
KMG And I’m Kara Meyberg Guzman.
SB: Thanks for listening to Santa Cruz Local.
TRANSCRIPT OF NEWS CONFERENCE
GAIL NEWEL: Good morning. Thank you to all of us who have joined us both virtually and in person. Again, I appreciate those who are wearing face coverings here in the room. I’m going to start as usual with our latest case numbers as – as of this morning, there are 98 known COVID-19 cases in Santa Cruz County. A reminder that there are many unknown cases as well, but we know of 98. This includes the two deaths, including the most recent death this week. I’m going to give you a breakdown of the data as of last night at 5pm, which includes 96 cases. 43 of those are male 53 female. Three are pediatric cases under the age of 18. 19 are over 65 with the remainder in the 18 to 64 age category. 17 of those have required hospitalization during their COVID-19 illness 41 have now recovered we’ve received 2460 negative a lab results. When you add her positive results to that we’re over 2500 lab tested knowns so far, a reminder that this does not include pending tests from commercial labs. We’re not privy to those numbers. So we don’t know those numbers until the results come back. Cases are spread throughout the county, with 32 in North County, 34 in Mid County and 22 in South County, with eight under investigation.
JASON HOPPIN: So now I’m gonna open it up for questions.
KARA MEYBERG GUZMAN: Hi, Kara Meyberg Guzman from Santa Cruz Local. This is a question I guess for Mimi: On Tuesday – at Tuesday’s Board of Supervisors meeting you shared a chart of all the projections up till May 1st for numbers of hospitalizations. Can you talk a little bit about how that chart factors into your decision making or into the leadership teams decision making about, you know, Shelter in Place Order type decision?
MIMI HALL: Sure. I think it’s important for the public to know that all of our decisions, whether it’s the timing for alternate care sites, or lifting of certain targeted portions of shelter in place, are driven by data. And early in the pandemic, we had very little data. So as we get more and more cases and more and more hospitalizations, it gives us a little bit more confidence in the data modeling that we’re doing. So we’re now running models every week. We were previously doing them at longer intervals, simply because we didn’t have the cases. With our weekly modeling, our last modeling was run on the data that we had April 11th and that disease curve shows that our surge, which we, we’ve kind of in it, we’ve named our benchmark for surge at 100 hospital beds. And so that mark was previously calculated to be April 14. And now it’s mid May to the range of the beginning of June. So what that does is it had us reassess we had called out for volunteer alternate care side medical and support staff. We’ve done a lot of things that now we have put on hold until later in the month, because we don’t want to have those resources here when they could be elsewhere. In terms of the shelter in place order, that data is really, really important to give us an idea of, especially Gail – working with the parks director, with law enforcement and the sales office to understand: what are the safest areas of shelter in place to start lifting. It’s important to note that we expect when we lift portions of that we’re going to start seeing more cases. So we talked last time also about testing capacity, we are ramping up our testing capacity. And so there – it’s not all or nothing. And so what we know right now is we have enhanced ability to test nearly 1000 additional tests just in the last couple of weeks. And what that tells us is: if we do small pocketed areas of shelter in place loosening, we have the ability to immediately test when we have those. I don’t think that we’re at the place and I don’t -and Dr. Newell can chime in as well, where we will have any kind of broad lifting of these because we don’t have the capacity to follow up should we have resumed outbreaks.
JASON HOPPIN: Please mute.
MIMI HALL: Would those on the phone please mute?
KARA MEYBERG GUZMAN: A follow up question to that. At Tuesday’s Board of Supes meeting you said that we need, for criteria, you know, more testing more PPE and more people power to do the tracing, more epidemiologists. How are we doing on those three areas?
VOICE ON PHONE: And if you could speak up a little –
MIMI HALL: Sure, sorry. OK. So in terms of more testing, we actually are ramping up our testing capacity. We have our commercial labs who have really shortened the length of time that they are responding back with test results. Some of the commercial labs a couple of weeks ago, were getting us results seven to eight days later. And now it’s more like two days, four days. So that’s a positive. The other positive is that we do have local testing available now through a few sites and one of those sites is our own county clinic. It’s important for people to know that those testing sites are for patients of those areas. I think that in the long term, there’s some thinking that we can do. And we’ve already started that thinking about how we can make the shift to community wide testing. We’re not there yet. But we don’t need to be there yet. We have to be ready for that place, maybe in a couple of months, and we start coming down the curve and thinking about how we’re going to further lift shelter in place. But that’s phased in. In terms of workforce, that’s another thing that we’ve been thinking about. Just as two weeks ago, we’re planning on workforce for alternate care sites. And we’re still on that plane. Now, we have to start planning for our workforce in three to six weeks from now and beyond. Because, again, if there is going to be any shift in the disease, perhaps related to any changes to shelter in place, we’re going to have the workforce and there is a robust system. A lot of different counties are actually starting to make plans for that. And we’re – we’re doing the same. What were the other things?
KARA MEYBERG GUZMAN: PPE?
MIMI HALL: Yeah, so PPE, there’s a little bit of good news. It’s not great news, but we do have – we’re receiving, it seems to be like weekly shipments from the state. And I hope that they continue and it’s not everything that we asked for, but they’re enough to get us by. We are still in something called contingency status. So the CDC for PPE has three statuses. One is conventional meaning you operate as normal, you follow all of the safety precautions you normally would. But then when scarcity begins, there’s contingency and crisis status. And so we are right now as a nation in crisis or in contingency status. So that means that we really have to preserve PPE across all different kinds of workers and we’re really encouraging the public and people who aren’t direct medical care service providers to not use medical grade PPE. One of the things that Dr. Newel has mentioned is – so what about the downside of the curve and having enough your question of broad testing, testing requires PPE. So to even get to that place where we think that we could, we have to get out of contingency status and getting out of contingency status means that we’re going to as a community have about a month’s worth of PPE stock on hand for the healthcare system.
KARA MEYBERG GUZMAN: Are any of those the limiting factor in terms of when we can start lifting some of the shelter in place?
MIMI HALL: No, I think the limiting factor is really – the biggest limiting factor is disease. We have got to see our cases and our hospitalizations start decreasing. So for those of you who think if we just get you all PPE if we just get you testing, I mean, that’s only part of the formula. We actually have to see the cases start decreasing.
DREW ANDRE (KION): Doctor. It’s now Thursday. What’s the status going forward for parks and beaches? What, basically – what will be back open and what won’t?
GAIL NEWEL: So as of midnight last night, all the beaches and parks reopened. So I hope our public will take advantage of those and enjoy their outdoor time. But it’s very important that the social distancing requirements be maintained. If we see large gatherings of crowds, we may need to close some or all of the parks and beaches again, I have left it up to local jurisdictions to determine if social distancing requirements are regularly breached. And if so, they have the right to close down areas of the parks for example, picnic table barbecue areas, or skate parks or dog parks. But as of midnight, the beaches and parks are open so I hope everyone can enjoy them responsibly.
DREW ANDRE: Overall, what led to your decision to open it back up or not extend it further.
GAIL NEWEL: Well, my intention was always to just close them for the seven days around the holiday weekend last weekend, knowing that we had many visitors from out of the area, and that traditionally folks gather on the beaches and in the parks for – to celebrate those holidays. And so now that we’re past that, I feel more comfortable giving it a go again.
JASON HOPPIN: Do we have a phone question?
NICHOLAS IBARRA (SANTA CRUZ SENTINEL): Yes. Nick Ibarra.
JASON HOPPIN: Go ahead.
NICHOLAS IBARRA: Okay, I’ll go so this is Nick Ibarra with the Sentinel, Dr. Newel and Director Hall. I’m wondering about the modeling and my question is: when you look at the actual rate that cases are increasing right now it seems to be very linear and at a pretty flat rate. And yet the modeling that you presented on Tuesday shows a significant increase in May. Can you talk about what would cause that inflection point? If there is an inflection point? Would it be the loosening of restrictions due to something else? And can you just help interpret why we would start seeing many more hospitalizations in mid May or early June?
MIMI HALL: It’s actually just math. So those models are based on inputs that go in. And so you calculate based on the current cases that you have in the current trend, a double time. And so if you know exponents in math, then the further along you get on your axis, the higher the increase. Does that makes sense? I don’t know.
GAIL NEWEL: It’s an algorithmic increase, which is what makes the curve. The other area Nick, that we’re really concerned about, is congregate living. So if for example, we had an outbreak and an outbreak is defined as two cases for COVID-19, if we had an outbreak within one of our congregate living settings, for example, a skilled nursing facility, it could spread very quickly within that facility. And so that can cause increasing numbers quickly within a community. So whether it be in a homeless population, in a jail, in a migrant housing situation, in a skilled nursing facility, numbers could increase quickly. And we need to be nimble enough and have the resources to respond quickly to those outbreaks.
MIMI HALL: And I do want to point out one thing about the modeling. Modeling is a prediction. It’s for – it, well, it depends on how you define prediction. It’s, it’s not this is a crystal ball into the future dependent on a lot of different things these are the possible scenarios. The most likely scenario is the middle ground, and there’s a 50% chance of the scenario up or down with the middle ground and then there’s a large swath of 95% credible interval that we get our best in worst case scenarios.
JASON HOPPIN: Something else from the phone?
NICHOLAS IBARRA: Jusst to quickly follow up with that. There is – my point is that actually looks like the doubling time right now is slowing. So would this model suggesting a second peak if the doubling time and slowly right now, then even understanding the exponential growth we – you know, on the current curve, we wouldn’t necessarily be looking at these numbers. So I’m just curious if you could explain what might lead us to think that that trend is going to reverse course.
MIMI HALL: Yeah. So if you, so one of the things is that our modeling only goes out several weeks. And so what we expect is that the peak is actually going to be later. So you don’t even see the peak on those models right now. So the slowing down that you’re seeing, I’m confident is a result of our very, very stringent Compliance and responsibility of the public and staying in line with this social distancing and children place orders. And so what we’ve done is flatten the curve so that you can’t see the peak anymore on the models that we provided. So as time goes by and we have more information, we can do some longer range modeling, but I would caution you to think that we’re at the peak now. We’re not. It’s just that the curve is so flat that you can’t see the top of the curve.
NICHOLAS IBARRA: Are you concerned that, that reopening the beaches, the Boardwalk, etc, coupled with the fact that you’re saying the curve has flattened will give people a false sense of we’re through the worst event and we could start going back to normal?
GAIL NEWEL: Well, let me clarify that the boardwalk is not open and I don’t anticipate that the Santa Cruz Beach Boardwalk will open this summer at all.
[Editor’s note: Newel later issued a statement saying that it’s too early to predict if the boardwalk will be closed this summer.]
There are no anticipated mass gatherings or really gatherings of any size for a long time to come. So I want to make sure that everyone understands that. When we talk about starting to lift some restrictions, we’re talking about very low risk activities. For example, outdoor activities such as allowing gardening and landscaping if social distancing requirements can be maintained. Or another example is, perhaps opening golf courses, again, with very specific social distance restrictions maintained.
JASON HOPPIN: Jondi?
REPORTER: [INAUDIBLE] from the Register Pajaronian newspaper over here in Watsonville. The cases, the number of cases in South County are the lowest throughout the county. Do – is there any specific reason or multiple reasons why that is the case? Can you give us an explanation for that?
GAIL NEWEL: I would guess that initially, this virus was brought into our country and our communities from commuters into the Silicon Valley for work and school, and in addition, international travelers, and that’s a population that lives more in Mid and North County. And I think the South County as a result has been relatively protected.
MIMI HALL: And I do I have a theory, an unofficial anecdotal theory that accompanies that because Monterey County now exceeds the number of cases that we have, and they have just as much agriculture if not more than us. My theory is that we have a significant population of immigrants and South County in a significant undocumented population. And there have been lots of things that have caused fear in that population, including public charge, ICE raids, and all of those things. So I feel like that population is used to staying at home. And now with shelter in place orders, when there are potentially people looking out for people being out and about, it could be a potential factor in keeping that population more at home and more out of the public eye. It’s just my theory, and that that may be helping with dampening the amount of spread in South County.
GAIL NEWEL: They may also, that population may also be more reluctant to get tested. So it could be that they’re that community is being under tested. Yeah.
MIMI HALL: I will add that we’ve got we have a huge growing season coming up. And that’s the next place that we have to turn our attention is how do we help the agricultural community when they’ve got agricultural workers and close quarters and everything, make sure that they’re following safe practices. And we have the ability to help them quickly as soon as the case is identified.
JASON HOPPIN: Jondi?
REPORTER: Do you know how many South County residents have been tested those, those 5000 cases? 2500 cases, I’m sorry.
GAIL NEWEL: I don’t have that number. I’m sorry.
JASON HOPPIN: Jondi.
JONDI GUMZ (TIMES PUBLISHING GROUP): You mentioned last week that there were healthcare workers infected. Do you have the numbers on that? And you know, whether your nurses or doctors or firefighters or whatever it is?
GAIL NEWEL: I know I promised to bring those today and my epidemiology staff is working on that but I don’t have that for you yet today. I know they showed me some rough numbers, but I wasn’t ready to reveal those yet. But I want to caution that even if we give you numbers of healthcare workers and first responders who have been impacted that that doesn’t mean that they were infected on the job. So they could have been infected elsewhere, outside of their actual work hours.
JONDI GUMZ: And as far as the congregate settings, are there any cases that have cropped up in the congregate settings?
GAIL NEWEL: Fortunately, at this time, we have not had any outbreaks in any of the congregate settings. I’m really impressed with the sheriff’s efforts to keep our jail population safe. So in all of our adult detention facilities, the census is much lower. There’s housing set aside for quarantine and isolation. Every single person employee visitor that who comes in is screened for a temperature check similar to what you all had, who are here in the room today, before they can come in. The jail has been closed down for a long time already for visitors except those required by law. Vendors are also checked before they come in. And any new newly incarcerated individuals are placed into a 14 day quarantine unit before they’re released into an individual – into the general population. So all of those measures have been really important to keep our jail population safe.
KARA MEYBERG GUZMAN: Can you talk a little bit more about what’s happening in the jail? Is there enough PPE for all the workers, for example, and is there enough — do you have enough testing to test even more than the people who are symptomatic?
GAIL NEWEL: We have – we’ve set aside PPE for the jail and the sheriff’s office, and we’re working with them to ensure that there’s adequate PPE and testing. I can’t say for certain depending on the size of an outbreak that could happen there. We’ve seen this to be a problem nationally and internationally in in incarcerated populations. So that’s one of the reasons that we’re working so diligently with the sheriff’s office to prevent outbreaks here.
JASON HOPPIN: Was there one on the phone?
REPORTER: [INAUDIBLE] Gail Newel, we know that you were working with the Association of Bay Area Health Officers, in conjunction with a number of other Health Officers all across the Bay Area, across the region, what did the collaboration look like? Will be talking about slowly reopening things, or allowing certain low risk activities to resume like you mentioned landscaping and gardening. What did that collaboration and decision making look like?
GAIL NEWEL: At this time, we’re meeting three times a week in a virtual meeting. And in addition, we communicate through an app called the Slack channel. Some of you may Be familiar with it. It’s used mostly for emergency response, but that allows us to share and post documents and orders and guidelines that we’re developing. In addition, we work with a statewide organization of Health Officers called the California Conference of Local Health Officers. And so I spend several hours a week with other Health Officers collaborating on next steps.
KARA MEYBERG GUZMAN: Follow up question –
REPORTER: Specifically in determining those next steps, what are some of the other activities or professions where we could begin to see these restrictions eased or lifted? You said earlier, I think like landscaping gardening, a lot of folks going to golf courses again, places where physical distancing can be maintained. What are some of the other considerations that important in the professions or activities.
GAIL NEWEL: I think if you use your imagination around what could be accomplished while still maintaining the social distancing requirements, then you can imagine what might be allowed to open. So there’s talk about other small businesses if social distancing can be maintained, perhaps resuming preventive health care and dental care. Perhaps day camps for children this summer, that’s going to be a big problem. And something that we’ve spent a lot of time talking about is, as the school year ends, even though the schools have been dismissed, there’s the childcare problems will continue through the summer. And as more businesses reopen, that’s going to become an increasing problem. So I’m – I’m working locally here with Parks and Rec and other entities as well, to help guide them on what could be developed using the current childcare guidance that’s in place on the current shelter in place for, and extending that to the K through 12 population for day camps for the summer.
JASON HOPPIN: Okay, let’s go in the back of the room here. We have one in the room. Sorry, hang out on the phone.
ASHLEIGH PAPP: Of the 98 confirmed cases here in the county are any most the homeless population in any specific updates there? I don’t think that we’ve had any cases among persons experiencing homelessness. I know that we are sheltering people in the first of several hotels that we intend to open. But those are the elderly and medically fragile folks from the homeless population. But I am pretty sure we don’t have any cases among the homeless.
JASON HOPPIN: And I have more info on facilities if you want to call it. Thank you.
JACOB PIERCE: This is Jake Pierce from Good Times. Now that the Association of Bay Area Health Officers is thinking about slightly expanding the list of essential businesses, what are some of the unintended consequences or impact of this level of shelter in place? And how are Health Officers thinking about those trade offs as they evaluate what’s next?
GAIL NEWEL: Well, the big one, and where you can all play a part is that when we talk about slowly beginning to lift shelter in place restrictions, that the general public can get very excited about it and think that everything’s going to resume quickly. And so you can help us by messaging that this is going to be a slow, long process. And restrictions are going to be – need to be lifted very carefully and slowly a bit at a time. And then restrictions may have to be placed back depending what we see on the disease – disease curve. So we really think that instead of one big curve, we’re going to see a series of ripples. So I’ve been saying, you know, instead of a tsunami, we’re going to have a series of ripples and asking Santa Cruz to ride the waves.
KARA MEYBERG GUZMAN: Mimi you said, you were planning for a surge of 100. Can you more explicitly define what that means? And I guess this is a question for Dr. David Ghilarducci: What is our hospital capacity? Like is 100 within our reach, I guess?
DAVID GHILARDUCCI: Yeah. Thank you for that question. So, we have been looking at some State projections. Currently, we think we have about 400 hospital bed capacity in the county that’s combined of three inpatient facilities. That number may vary a little bit depending on certain conditions. We have about maybe 45 to 49, ICU or ventilator capacity beds. The projections are that State projections at least released recently suggests that Santa Cruz may experience – most likely experience about 300 hospitalizations at peak. So bed supply of 400, 300 at peak, we should be okay there if it goes as, as most likely. Obviously, these are broad curves and there are many possibilities. I’m a little more concerned about ICU capacity. And I’ve mentioned that before here. They’re projecting that we may need up to 100 ICU or ventilator beds at time of peak and as I said, we have less than half of that. So we’re working very hard to find ways to expand capacity and that would include moving patients to where – to other counties where ventilators may be and so very fluid situation.
KARA MEYBERG GUZMAN: Well, is that, that regional help, is that enough to meet those 50 extras?
DAVID GHILARDUCCI: Yeah. That’s a great question. Now in a normal time, you know, we can, we can safely rely on outside hospitals to provide extra help. During this pandemic, we are not assuming that that will be available. So, we have to look for internal resiliency to the extent that we can. And so that’s going to probably mean some real creative solutions. You know, getting ventilators from the state or the feds would be helpful, finding people to staff, those ventilators, the medical professionals that you need to provide that intensive care. There’s other things that ICU patients need besides just the ventilator itself. There’s lots of medications that they could have six or seven medications, infusing at one time for very, very sick people. So lots of labor involved there. And so the people part of it will be important as well.
DREW ANDRE: We see many outbreaks in nursing homes around the country. I know you guys have mentioned that there, there is a team within your group that’s focused on that what specifically is being done to prevent an outbreak in one of our local nursing homes?
GAIL NEWEL: I’m really proud of our communicable disease teams. They’ve been personally going out on site visits, Epidemiologist, public health nurses case investigators, and working very proactively with our skilled nursing facilities. So they’re helping assess PPE supplies and need for the future, they’re mapping they’re doing actual mapping of facilities to help facilities decide how to best cohort housing for isolation and quarantine. They’re working to educate staff and managers and owners of the skilled nursing facilities on how to best care for COVID 19 patients, and they’re doing all this with an ongoing relationship that they already have with these skilled nursing facilities because they work with them already managing outbreaks of things like flu, shigella, tuberculosis. So it’s, it’s a an established relationship that that is being used to the best advantage for everyone.
REPORTER: [INAUDIBLE] no outbreak we know in the nursing facilities. Have there been any cases at all though many nursing facilities?
GAIL NEWEL: We had one healthcare worker in the who worked in a skilled nursing facility, but we did surveillance testing with, in that facility and found no cases at all.
DAVID SERRANO: Just to get back to the beaches real quick. With the beaches being open, what’s the one message you really want to get across to the local people and to the people over the hill that say, hey, the beaches are open. What – what is it you really want to get across?
GAIL NEWEL: Ideally, people would use the outdoor areas that are in their own neighborhoods, so we don’t have too much intermingling within communities or neighborhoods because that’s how disease spreads. So for example, San Mateo County has a limit that people shouldn’t go beyond five miles of their home to exercise. Other communities say, well, you really shouldn’t go anywhere that you can’t walk to from your own home. We’ve decided not to put those kind of limits as a legal order, but it’s best to stay within your own neighborhood for your outdoor activities. The most dangerous activity is, is to gather in crowds, so spent – being within six feet of non household members for a prolonged period of time. So greater than two hours is at most risk greater than 10 minutes already puts folks at a moderate risk. So gatherings are what’s really dangerous in our outdoor areas.
REPORTER: You don’t want people to hear Santa Cruz beaches or [INAUDIBLE] flooding over the hill again.
GAIL NEWEL: I’d love to say that. But we, our neighboring counties provide us with a lot of benefits as well. We need to acknowledge that it’s a two way street that many of our community members work or go to school in our neighboring counties, and we don’t want to just shut them out. We’re not going to do that at this time.
JONDI GUMZ: You mentioned that the Wharf to Wharf organizers should plan on 2021. What about the popular Junior Guards program where kids are learning their life saving skills, is that’s something that didn’t happen this year?
GAIL NEWEL: If, if the Junior Lifeguard program happens this year, it will look different than it has in previous years. In previous years, it’s so cute. I love seeing the crowds of kids out on the beach, but it just can’t happen that way this year. So we’re working with County Parks and Rec and other agencies to try to figure out ways that we can make the usual summer outdoor activities happen but in a different way.
JASON HOPPIN: Alright, Nick, go ahead.
NICHOLAS IBARRA: Yeah, so my question relates to the business community and on Tuesday, there was mention made of that being a factor in looking at what, what restrictions to lift and just how your office is looking at the orders. Can you talk more about the dialogue that’s happening, if any, with business folks, and how that is forming your decisions, if at all.
GAIL NEWEL: A lot of my decisions also rest with the state because I can’t lift any kind of restrictions the state has put down. So the governor has a Shelter in Place Order of his own. And I can’t do anything to make those less restrictive. I can make them more restrictive but not less. So a lot of what happens here locally depends on what the governor decides to do statewide. On Tuesday, he held a press conference, and he outlined his six criteria for lifting restrictions. So I would refer you back to those. And then we’ll, we’ll have to tailor local restrictions based on that guidance. And if anything, we could make them tougher but not looser.
NICHOLAS IBARRA: But in your dialogue between your office and the business community, can you talk about what that dialogue is and who you’re talking with at this point, if anyone?
GAIL NEWEL: Our environmental health unit, and regularly visits and communicates with all of the areas, restaurants and other businesses that sell food. And I know some of our other, like our cannabis unit also works with the cannabis industry. So they have been working very closely about making plans to continue to operate in – under current circumstances and will work with them for the future. Beyond those, the food and cannabis, I have not worked directly with businesses.
JACOB PIERCE: This is Jake from Good Times. My second question is, is a follow up for Dr. Ghilarducci -about the point of ventilators. We’ve heard a few times that total capacity total ICU and ventilator capacity, it sounds like a little bit under 50. Does that mean that the county has less than 50 ventilators total?
DAVID GHILARDUCI: Yeah, the capacity that I referred to has to do with, with space in the hospitals as well as the number of ventilators. But that’s correct. We have less than 50 ventilators. There are a handful of other options like anesthesia machines and things like that that could be employed but our operational capacity is is a little bit less than 50.
JACOB PIERCE: In each of those ventilators, how many times can those be reused? Or how easy is it to refurbish them? Or is the expectation that each would only be used once?
DAVID GHILARDUCCI: Great question, these ventilators can be used multiple times they have to be decontaminated. There’s a process for that. There is a possibly a small cache of what we call disposable ventilators. These are gas powered, they’re not gasoline powered but powered by compressed air or oxygen. That are one time use. I don’t know exactly how many of these are present. One hospital has a small supply. But that said, without the people to run the ventilators, that’s the other limitation that we’re facing.
DAVID SERRANO: What about CPAP machines would that be able to be used as an alternative for like my mild case of coronavirus?
DAVID GHILARDUCCI: It has to be a very mild case. Usually when people get to the point of respiratory distress where they need to be intubated, CPAP would probably not be it usually in the hospital. It’s called BiPAP but essentially the same thing would not really be an option.
KARA MEYBERG GUZMAN: How many epidemiologists does the county have on staff and how many more would be needed to have the people power to track cases? All the cases.
MIMI HALL: I see Corinne counting on her fingers. Looks like we have five full time FTE epidemiologists. We also have a couple of part time ones and one actually is working remotely from Amsterdam. And so we pull into the resources that we need. One of the things that we’ve done during this pandemic emergency response is pulling all different kinds of stuff. So we pulled in a couple of different epidemiologist. And if we need to pull in more we can do that. We actually put in a request right now, one of the ways that we’ve gotten some excellent epidemiologists, is through a state program that the state actually pays for a portion of an epidemiologist salary to come work for us for a period of time. So we have we make that request annually, and we have another request going forward, I believe it’s next month.
GAIL NEWEL: We, we have just been notified that we are getting two tomorrow. Yay, we’re getting to additional epidemiologists.
KARA MEYBERG GUZMAN: And how many more are needed to have, have enough people power to track?
MIMI HALL: Well, I mean, that’s just such a loaded question. It’s kind of like how much money do you need? I feel like we have great capacity with our epidemiologist right now. And they have good partnerships with colleagues in other institutions as well. So I think that we need person power in a lot of different areas. We’re able to keep up with the tracking and the modeling and the data input. Some other areas it’d be really great to have staff is, so when we move away from where we are, and we’re going to look at this long term mitigation it would be really great to have people who are great at data. And by data, I mean, data embedded in health information exchange, to pull surveillance information, symptomatic information, data to the public so that we can use apps on our phones so people can self report. So those are all the things that would be really great for us to build the capacity to do. We’re looking into some of those things, but it really can’t be a Santa Cruz effort only and we don’t live in a bubble. So the things that we would like to do, there really has to be a regional or statewide approach, preferably national, but I don’t know if we’ll get there.
JONDI GUMZ: Is there a possibility of working with the local company Looker, that’s part of Google their expertise is data science.
MIMI HALL: Yeah, actually, there is. If we do go into using the apps, it’s – I can’t remember the name of the Google app, but that’s the one that you prefer for public health. And that’s publicly available to local health jurisdictions in the states as well.
GAIL NEWEL: Can we talk a little bit about face coverings? So we are moving toward more and more encouraging the use of face coverings. There’s not a lot of science behind the use of face coverings, but we do know now that COVID-19 is spread almost exclusively through large droplets, then those are the kind of droplets that happen when we sneeze, when we cough, when we talk. And so what we are assuming is if that we wear masks, cloth masks, or face coverings, we’re trying to call them, that the acceleration of those large droplets will be slowed by the mask that we’re wearing. So the mask does not protect you against disease. It does not protect the wearer against disease. It protects other people from the wearer. So thank you to all of you in the room who were wearing your masks and protecting the rest of us in the room. So it – because we’re still in a contingency with our PPE. Medical masks should not be worn by the general public. Those need to be reserved for health care workers on the front line. And so we’re asking the public to wear cloth face coverings whether it’s a handmade mask or a gator or a scarf or bandana tied around your face, to help protect others from you. And that’s because we know now it’s become clear that we’re able to infect others before we know ourselves that we’re infected before we show signs of being infected. So, if you can emphasize that to the public when I’m out and around in Santa Cruz, which is not a lot, but when I have been out and around, I’m not seeing great uptake of the masks. And I’m especially concerned about our elderly and medically vulnerable, that they seem to be not heading the social distancing requirements as much as others and so I’m encouraging everyone to add face coverings to the list of things that were already asking you to do. And I know it’s boring. So I’m going to go over those one more time. So, the social distancing requirements are four things. The first is stay home if you’re ill, if you’re showing any influenza like symptoms any upper or lower respiratory symptoms, stay home. And the second is to shelter in place, stay home as much as possible, you should only be leaving for essential activities, or for some outdoor recreation. And the third is wash your hands frequently with soap and water soap and water is preferred to hand sanitizer. A good 20-second scrubbing. If you don’t have soap and water available, use your hand sanitizer, and the fourth is to cover your coffin sneeze. And then if it’s with the tissue, discard that tissue right away. And don’t sneeze directly into your hands. That’s the most common way to infect people his hand – or infect yourself is from your own hands to your mouth, nose and eyes. Yeah, and the distance six feet distance.
ERICA MAHONEY (KAZU): This is Erica, so I’ve been curious. I think we’re gonna hear more from the governor in a couple of weeks. But as we look toward the summer, what constitutes a large gathering? Like what number of people would that be? This is kind of a personal question because I have a wedding.
GAIL NEWEL: Yeah, you need to think about moving the date of your wedding. I’m sorry to say it’s a heartbreak. I know I had to work with my niece on her wedding. At this time, the acceptable gathering size is zero, except for household members. The only other gathering that we’ve given our blessing to is for funerals, gatherings up to 10 people. Other than that, there’s no acceptable size of gathering of non household members.
ERICA MAHONEY: How about late June, do you think that would be –
GAIL NEWEL: We might, we might go to gatherings of 10 by late June, but that would be a very small wedding. I’m so sorry.
STEPHEN BAXTER: Are we all invited?
SOMEONE: Congratulations.
GAIL NEWEL: Yes, hardy congratulations.
ERICA MAHONEY: Thank you, thank you so much.
DREW ANDRE: I have one about the face covering: How how often should you be washing the cloth?
GAIL NEWEL: A quick answer about face coverings. It’s recommended to keep your face coverings clean washing them at a minimum of once a day.
REPORTER: I had a question about the statistics I know the county has the, the website that is updated, which is nice to have. And then there’s the CHHS database that has further breakdown with the ICU cases. And sometimes they’re not the same. It’s, you know, it’s interesting, like what you know, one time, counties say, oh, there’s, you know, so many hospitalizations. And then the state is saying, no, it’s this number of hospitalizations, and they’re saying some are suspected. And so we’re confirmed and then the suspected ones disappear. How, who manages that?
GAIL NEWEL: The hospital data dashboard that’s from the state, they get their data directly from the hospitals so the hospitals are required. The three hospitals here in Santa Cruz County are required to report every day to the state. And their data does lag behind for several days. And things like we’ve noticed like bed availability that depends a lot, not just on the number of beds or the number of ventilators. But it depends on staffing. And that can change hour by hour, literally not just day by day, depending on how many staff have called in sick, how many need to attend to their children, is it a holiday weekend, all of those kinds of things. In general, the case counts: ours are pretty much up to date every single day, by the time they’re posted. This date generally likes a little bit behind us.
REPORTER: In terms of hospitalizations, so we have a couple of different numbers that we post. We post ever hospitalized, and so if you’re looking at that it looks like a higher number than what the hospitals are saying. And then when they post suspected hospitalized, there was one weekend where there was some crazy number of suspected and all of them came back negative. So they’re putting in everyone that they suspect, but once the tests come back, then that number like dramatically goes down.
JASON HOPPIN: A couple minutes. Is there another one on the phone?
JACOB PIERCE: Yeah, I was wondering is when, so is it – quick two parter: So I’m wondering, Dr. Ghilarducci, if you can – you mentioned the 300 peak hospitalization number. When is the state projecting that? And as the second part, Dr. Newel, you talked about ripples, you know, instead of one wave, are we beyond the downside of the first ripple right now with the rate slowing, or should we be looking at it differently?
DAVID GHILARDUCCI: Well, it takes, first question, probably late May, early June.
GAIL NEWEL: And the second question, it’s too early to tell.
JASON HOPPIN: That was quick but let you have that one. Steven and go ahead.
REPORTER: Wondering if the doctor could tell me if they – are going to – are there any thoughts to re-closing beaches and parks for the Memorial Day holiday or is that too far out.
GAIL NEWEL: I haven’t even thought about that one yet. I have been worrying about Fourth of July. That’s always a problem. And there have been times years in the past where beaches have been closed for Fourth of July. Thanks for reminding me about Memorial Day. One more thing to add to my list of worries.
JASON HOPPIN: Anything else in the room?
KARA MEYBERG GUZMAN: Two quick questions. Are you worried about 4/20? And are can you share any more specifics beyond what’s on the county website about where in the county – so you’ve posted like North County, Mid County and South County, can you share any more specifics about where confirmed cases are or details on that?
GAIL NEWEL: I’m going to answer the second question first and say that we do have a breakdown by city but in some of the cities or towns, the numbers are so small that they don’t meet our threshold for medical privacy purposes. So we’re not ready to do that yet.
And then 4/20, I really think that I trust our community to do the right thing. And our community has done so well to date. And I want to encourage everyone to keep up the good work. And it’s because of all of you and your willingness to follow this social distancing requirements that we’ve had this kind of success. So I need to get to –
JONDI GUMZ: What about the grocery store workers? There’s a lot of concern about grocery store workers getting infected. Have there been any cases in that population?
JASON HOPPIN: Kill the phone. Sorry about that.
GAIL NEWEL: I don’t think so. No, I don’t.
JASON HOPPIN: Thank you, everyone.
EVERYONE: Thank you.
Stephen Baxter is a co-founder and editor of Santa Cruz Local. He covers Santa Cruz County government.
Kara Meyberg Guzman is the CEO and co-founder of Santa Cruz Local. Prior to Santa Cruz Local, she served as the Santa Cruz Sentinel’s managing editor. She has a biology degree from Stanford University and lives in Santa Cruz.






