Santa Cruz Local offers its news stories free as a public service.
We depend on people like you — we call them our Santa Cruz Local members — to chip in $9 a month or $99 a year to make sure vital information can be available to all. Can we count on your help?
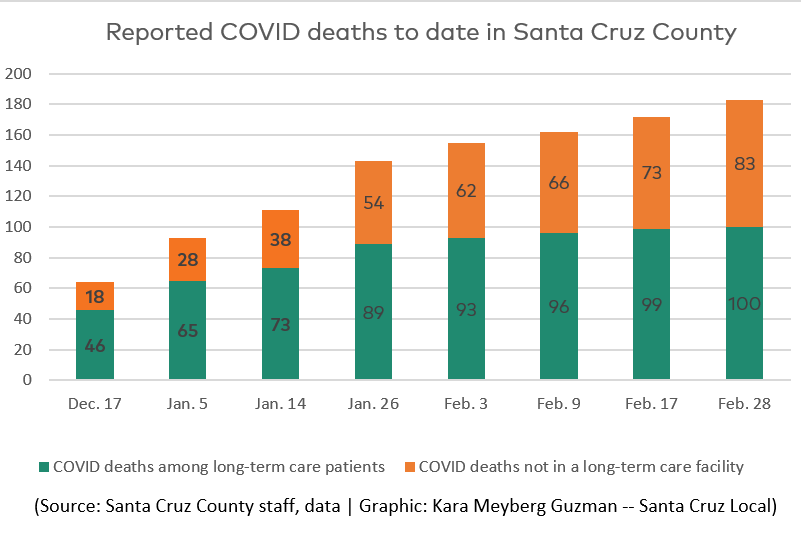
SANTA CRUZ >> Most of the 183 Coronavirus deaths in Santa Cruz County have been among residents of senior care facilities, yet many of those residents did not receive vaccines in December and early January as other groups did in part because of a lack of coordination among state, county and pharmacy vaccine providers.
From Jan. 26 to Feb. 28, 11 COVID-related deaths were reported among residents in long-term care facilities in Santa Cruz County. Some of those deaths might have been prevented if residents of those facilities had been more prioritized for vaccines, a Santa Cruz Local investigation has found.
Coordination was partly to blame. State leaders told Santa Cruz County health officials to allow a federal pharmacy program run by CVS and Walgreens to handle vaccine distribution at nursing homes and assisted living facilities in Santa Cruz County. County health leaders said vaccine supply was too limited to allow the county to assist.
Some recent deaths in long-term care facilities “may have been prevented by a quicker rollout,” Santa Cruz County Health Officer Dr. Gail Newel said Feb. 25.
“It would be a handful of deaths. But of course, every life is important, every death is important. So, you know, if that [federal pharmacy] program would have happened more quickly, more efficiently, then perhaps some of those could have been avoided,” Newel said.
When asked why it took weeks to schedule and administer vaccines at senior facilities in January, a CVS representative said the state only allowed the pharmacies to administer vaccines to skilled nursing facilities Dec. 28 and assisted living facilities Jan. 11. Santa Cruz County could have opted out of the pharmacy program, but county health leaders said they didn’t have the staff and the county would not have been reimbursed for vaccine distributions at senior facilities.
Meanwhile, the vulnerable residents of those homes — and scrambling administrators — were left to wait.
“It was really frustrating, because we had been told vaccines were coming,” said Joanne Simpson, office manager of Valley Haven Assisted Living in Live Oak. COVID-19 was a contributing factor in one death at Valley Haven since mid-December, according to county health data. “We had signed up for the federal (pharmacy) program,” Simpson said, “But then it was radio silence for quite a long time.”
Simpson said her pharmacy contact told her to keep looking for an email that set the date of Valley Haven’s first vaccination clinic. “Honestly, people are just making this up as they go along,” she said. “We were constantly checking to see if it had gone to spam.”
By the numbers
In Santa Cruz County, 100 of the 183 reported deaths related to COVID during the pandemic have happened in long-term care facilities, according to the county health department as of Feb. 28. A COVID death means it has a “county-issued death certificate that lists COVID-19 as a contributing or causal factor within Santa Cruz County,” according to the county health department.
Vaccine delivery schedules varied widely at long-term care facilities in Santa Cruz County. At places like Santa Cruz Post Acute in Live Oak — where 20 residents died of COVID-related causes, vaccines were first received Dec. 29. Residents at Valley Haven Assisted Living in Live Oak first received vaccines Feb. 4 — more than a month later, leaders there said.
At Sunshine Villa in Santa Cruz, the first doses of vaccine were received on Jan. 25. “There’s not much we could really do,” said Drayah Baylor-Reed, the business office director at Sunshine Villa. “We just patiently waited.”
Reported COVID-related deaths at Sunshine Villa grew from zero on Jan. 14 to seven by Feb. 17, according to county data. It can sometimes take two to three weeks to confirm a death is COVID-related.
There are roughly 90 long-term care facilities in Santa Cruz County. Santa Cruz Local contacted the 20 facilities with reported COVID-related deaths. Seven of these facilities are “skilled-nursing facilities,” also known as nursing homes, with residents that require more serious care. The 13 others are assisted living facilities.
At stake for the nursing home residents and staff was not just potential COVID transmission while they waited for vaccines. Many residents have not been allowed in-room visits with loved ones since the pandemic started. Isolation and low morale have been challenges, especially as they know others such as health care workers have received inoculations because of state rules.
“In the year that we’ve been doing this, we have definitely seen residents that used to be bright and shiny and happy decline dramatically in their illnesses,” said Erin Rose Wiley, an administrator for the residential care facility Paradise Villa in Live Oak. “There’s nothing I can do. It’s just sad and depressing,” she said.
While Paradise Villa staff still enforce strict pandemic protocols to try to keep residents safe, Wiley said some vaccinated residents can now eat communally at a social distance. “Socialization and community is a big deal,” Wiley said.
Reported COVID deaths to date in Santa Cruz County
| Facility | Jan. 14 | Jan. 26 | Feb. 9 | Feb. 17 | Feb. 24 |
|---|---|---|---|---|---|
| Aegis | 3 | 3 | 3 | 4 | 4 |
| De Un Amor | 0 | 2 | 2 | 2 | 2 |
| Dominican Oaks | 2 | 2 | 2 | 2 | 2 |
| Driftwood | 0 | 1 | 2 | 2 | 2 |
| Hanover Guest Home | 0 | 2 | 2 | 2 | 2 |
| Hearts & Hands | 7 | 7 | 8 | 8 | 8 |
| Maple House I | 3 | 3 | 4 | 4 | 4 |
| Maple House II | 1 | 1 | 1 | 1 | 2 |
| Montecido Manor | 3 | 3 | 3 | 3 | 3 |
| Pacific Coast Manor | 14 | 14 | 14 | 14 | 14 |
| Paradise Villa | 1 | 1 | 1 | 1 | 1 |
| Rachelle’s Home 1 | 0 | 1 | 1 | 1 | 1 |
| Rachelle’s Home II | 0 | 1 | 1 | 1 | 1 |
| Santa Cruz Post Acute | 20 | 20 | 20 | 20 | 20 |
| Sunshine Villa | 0 | 5 | 6 | 7 | 7 |
| Valley Convalescent | 3 | 3 | 4 | 4 | 4 |
| Valley Haven | 0 | 0 | 1 | 1 | 1 |
| Watsonville Nursing Center | 0 | 3 | 3 | 3 | 3 |
| Watsonville Post Acute | 16 | 16 | 17 | 18 | 18 |
| Westwind Memory Care | 0 | 1 | 1 | 1 | 1 |
| Total deaths in long-term care facilities in Santa Cruz County | 73 | 89 | 96 | 99 | 100 |
| Total COVID deaths in county | 111 | 143 | 162 | 172 | 183 |
Vaccine allocations
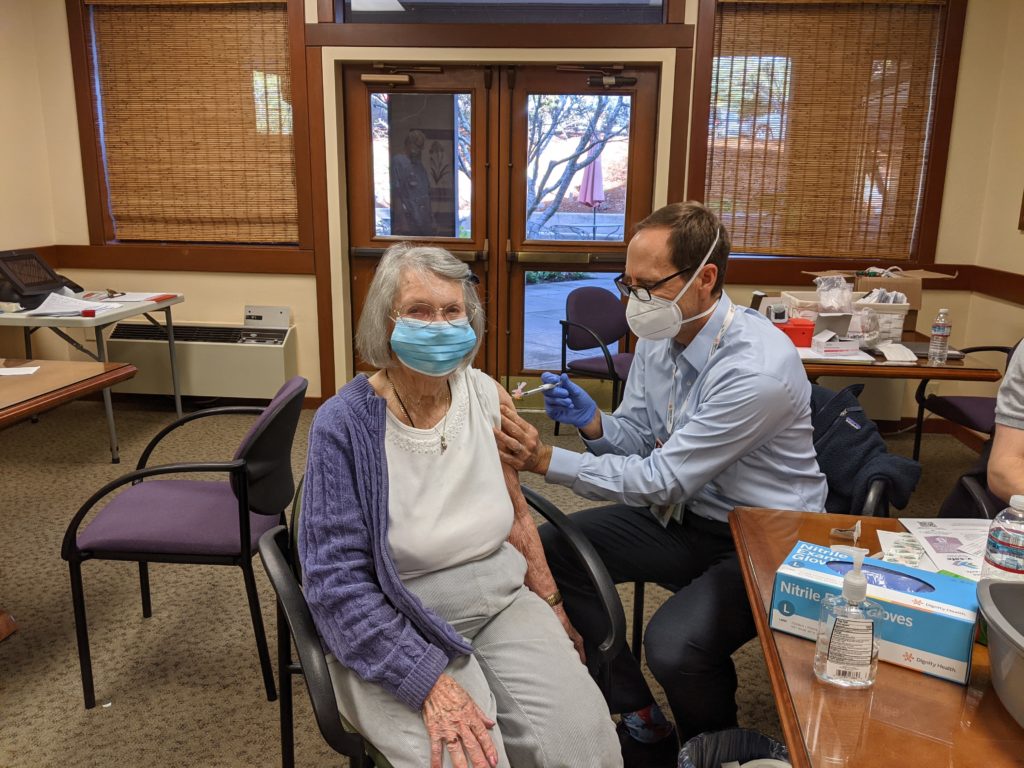
Health care workers and residents of long-term care facilities belong to the highest priority tier, according to California’s vaccine distribution plan.
Vaccinating vulnerable people in long-term care facilities is more complicated than vaccinating health care workers. Pharmacy workers who administered vaccines at nursing and assisted living homes had to work around the existing health care needs of residents who may have medical problems such as dementia. Staff and residents also aren’t required to receive the vaccination, so some opted out. The paperwork and logistics have been challenging, long-term care facility leaders said.
Vaccination clinics in long-term care facilities also require a “mobile strike team” of health care workers to administer the vaccine. The county health department did not yet have the capacity to form these teams, said Deputy Health Officer Dr. David Ghilarducci in a Jan. 14 interview.
Different programs supply vaccines for different groups. The California Public Health Department provides vaccines to the county health department, which then supplies health clinics that serve underserved communities such as Salud Para La Gente and Homeless Persons Health Project. California Public Health also distributes vaccines to large medical systems such as Sutter Health, Kaiser and Dignity Health.
In Santa Cruz County and across the nation, leaders of most long-term care facilities opted into a federal partnership with CVS and Walgreens called the Pharmacy Partnership for Long-Term Care Program to receive vaccines for residents.
The federal pharmacy program was intended to fast-track vaccinations to the most vulnerable people in nursing homes and assisted living facilities. Federal authorities announced the program in November, roughly a month before vaccines were available. On Dec. 13, Alex Azar, then the Health and Human Services secretary, said, “We could have every nursing home patient vaccinated in the United States by Christmas.”
It didn’t happen. In Santa Cruz County, the federal program has lagged behind the county’s own vaccination program, county health leaders said.
Vaccine deliveries delayed
Though the county’s first inoculation was on Dec. 16, the earliest nursing home vaccinations through the federal program didn’t occur anywhere in the state until nearly two weeks later, on Dec. 28. CVS representatives said the state did not allow those vaccinations until then.
Vaccinations for assisted living facilities occurred even later. Some facilities did not receive a first dose of vaccine until early February, nursing home administrators told Santa Cruz Local.
- Santa Cruz Post Acute received its first round of vaccines on Dec. 29 — one of the earliest in the county — which enabled it to receive booster shots Jan. 19. Rusty Greiner, an administrator at the facility, said it was a relief. Twenty residents of Santa Cruz Post Acute died from COVID-related causes during the pandemic — the highest of any facility in the county.
All 20 deaths of Santa Cruz Post Acute residents occurred before the first week of January, according to county data.
“I now live with an assurance that we can protect our residents that much more,” Greiner said. “I find great comfort in that.” He noted that Santa Cruz Post Acute still enforces strict pandemic precautions such as social distancing and masking. “We should be protected from a large-scale outbreak,” he said.
- Dominican Oaks, a Live Oak retirement community and senior care facility owned by Dignity Health, received its first vaccines Dec. 31. The vaccines came from Dignity Health’s share, not the federal pharmacy program, a Dignity Health spokesman said.
Why the wait?
Pharmacy leaders, county health officials and nursing home administrators tell different stories about why it’s taken so long to inoculate the people seemingly most at risk of COVID related death.
Santa Cruz County health officers said publicly in December that nursing home vaccine distribution was being handled by the pharmacy program. Ghilarducci, the county’s deputy health officer, said Jan. 14 that he was “frustrated” by the federal program’s “slow rollout” to nursing homes and assisted living facilities. He said county health leaders decided not to assist with vaccine supply in part because the state would not reimburse the county. Supply was limited.
“We unfortunately have to make this decision, if we do go ahead and do it ourselves, that we are OK with losing that vaccine and not having it available elsewhere,” Ghilarducci said. “So the vaccine that gets allocated to them is essentially lost to us.”
The slow start is one reason why Los Angeles County opted out of the federal pharmacy program for their skilled-nursing facilities, believing they could allocate vaccines themselves more efficiently.
Newel, the Santa Cruz County health officer, said that by the time the county had access to the vaccine in mid-December, all seven skilled nursing facilities had endured outbreaks, which played into her decision not to assist with vaccine supply.
“The vast majority of the nursing home residents and all of the nursing homes were already infected and had immunity that we knew would last for 90 days,” Newel said.
“If we had given away 3,000 or so of our vaccines for the community, that would have meant 3,000 (county residents age) 75-plus that wouldn’t have gotten their vaccine,” Newel said. “So there may have been deaths in that group as well,” Newel said Feb. 25. “These decisions are really difficult.”
The federal pharmacy program operates independently from the county. It answers to federal and state officials with little local oversight.
In October, long-term care facilities were surveyed on which pharmacy they preferred. They were also offered to opt out of the pharmacy program and work with local clinics directly. The vaccines from Moderna and Pfizer require two doses: the initial vaccination shot, and a second booster shot three to four weeks later.
Pharmacy representatives visited each care facility three times with a three-week delay between visits, CVS representatives said. The third visit was to provide booster shots for anyone who missed the first clinic and received their first dose at the second clinic.
State leaders mentioned the pharmacy program timeline publicly. But it’s unclear why the program wasn’t authorized to begin earlier — when the first vaccinations in Santa Cruz County occurred on Dec. 16. Also unclear is why the earliest start date for nursing homes was Dec. 28 and assisted-living facilities Jan. 11, even though they belonged to the same high-priority tier.
Frustration at senior homes
In Santa Cruz County, many leaders of senior care facilities said they didn’t know those dates and expected vaccines sooner. Some felt left in the dark, administrators told Santa Cruz Local.
At Hanover Guest Home, an assisted living facility in Santa Cruz, administrator Stephanie Means said she and others “worked for two months to get [the vaccine] here.”
During a Feb. 22 interview, Means said she was preparing her residents for second doses that day. She said facilities like hers should have been on the top of the list. Hanover has had two COVID-related deaths since mid December, according to county health data.
“We could’ve maybe avoided a death, but that is uncertain,” Means said.
Just as many assisted-living facilities in Santa Cruz County were anticipating their first vaccines the week of Jan. 25, the county expanded its own vaccine distribution to qualifying residents aged 75 and older.
Most nursing homes with COVID deaths in Santa Cruz County did not return multiple requests for interviews, including Watsonville Post Acute — where 18 COVID-related deaths have occurred since the start of the pandemic — and Pacific Coast Manor in Capitola where there have been 14 COVID-related deaths in 2020, according to the county health department.
Pharmacy representatives respond
The two retail pharmacies charged with the vaccine rollout to skilled nursing homes and assisted living centers in Santa Cruz County were Walgreens and CVS.
A Walgreens representative denied any delays in vaccine distribution in Santa Cruz County. The pharmacy has completed its first rounds of vaccine clinics for 324 skilled nursing facilities in the state, according to Walgreens data as of March 1. Walgreens also handles 1,581 assisted living facilities. It plans to finish vaccine distributions by mid March.
Walgreens declined to say how many nursing homes or assisted living facilities received vaccines through January.
A CVS representative, Monica Prinzing, said the rollout was on schedule.
“Criticism that our long-term care COVID-19 vaccination program is slow or behind schedule in the state of California, including Santa Cruz County, is not accurate,” Prinzing wrote in an email to Santa Cruz Local. “We remain on target within the program parameters, as agreed to by the state.”
TIMELINE
| October 2020 | Federal authorities announce the Federal Pharmacy Partnership for Long-Term Care Program. |
| Dec. 13 | “We could have every nursing home patient vaccinated in the United States by Christmas,” says Alex Azar, then secretary of U.S. Health and Human Services. |
| Dec. 16 | First vaccine doses administered in Santa Cruz County, to health care workers. |
| Dec. 25 | Christmas |
| Dec. 28 | First nursing home residents in California receive vaccine. |
| Dec. 29 | Santa Cruz Post Acute residents first receive vaccine. |
| Dec. 31 | Dominican Oaks residents receive vaccine, administered by Dominican Hospital. |
| Jan. 11 | First assisted living facilities in California receive vaccine. |
| Jan. 13 | Driftwood Healthcare Center residents receive vaccine. |
| Jan. 15 | Sutter Health clinics in Santa Cruz County begin vaccinating Sutter patients 75 and older. |
| Week of Jan. 18 | Dignity Health Medical Group-Dominican and Kaiser Permanente began vaccinating patients 75 and older. |
| Jan. 21 | Paradise Villa residents receive vaccine. |
| Jan. 25 | Sunshine Villa residents receive vaccine. |
| Week of Jan. 25 | Residents 75 and older who are patients of Salud Para La Gente, Watsonville Health Center, Homeless Persons Health Project, Emeline Health Center begin receiving vaccine from the county. A county-run clinic begins vaccinating people 75 and older in ZIP codes 95019, 95076 or 95077. |
| Jan. 14 to Feb. 3 | Confirmed COVID-related deaths among residents of Santa Cruz County long-term care facilities grows from 73 to 93. It can sometimes take two to three weeks to confirm a death is COVID-related. |
| Feb. 1 | Hanover Guest Home residents receive vaccine. |
| Feb. 2 | De un Amor residents receive vaccine. |
| Feb. 3 | Aegis Living Aptos residents receive vaccine. |
| Feb. 4 | Valley Haven residents receive vaccine. Sutter Health begins vaccinating patients 65 and older in Santa Cruz. |
Because the state allowed CVS to administer vaccines in skilled nursing facilities Dec. 28 and long-term care facilities Jan. 11, CVS performed as asked by state health officials. CVS representatives on Jan. 6 promised first doses within three to four weeks of those start dates and delivered.
The state tasked CVS with vaccine distribution to 499 skilled nursing facilities and 14,557 other long-term care facilities in the state, according to CVS. CVS has completed 99% of second doses in skilled nursing facilities, and 99% of first doses in assisted living facilities as of late February, Prinzing wrote.
It’s not clear what percentage of facilities in Santa Cruz County or the state were completed through January.
Prinzing wrote, “We’re in regular communication with our facility partners, and they can contact us with any questions or concerns.”
Kara Meyberg Guzman contributed to this report.
Correction: An earlier version of this story misstated the name of the Pharmacy Partnership for Long-Term Care Program.